
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Influenza A virus
Medical expert of the article
Last reviewed: 06.07.2025
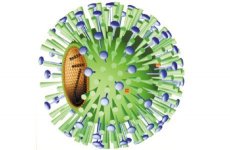
Influenza A virus is a virion that has a spherical shape and a diameter of 80-120 nm, its molecular weight is 250 MD. The genome of the virus is represented by a single-stranded fragmented (8 fragments) negative RNA with a total molecular weight of 5 MD. The nucleocapsid symmetry type is helical. The influenza virus has a supercapsid (membrane) containing two glycoproteins - hemagglutinin and neuraminidase, which protrude above the membrane in the form of various spikes. Hemagglutinin has a trimer structure with a molecular weight of 225 kD; the molecular weight of each monomer is 75 kD. The monomer consists of a smaller subunit with a molecular weight of 25 kD (HA2) and a larger one with a molecular weight of 50 kD (HA1).
The main functions of hemagglutinin:
- recognizes a cellular receptor - a mucopeptide containing N-acetylneuramine (sialic) acid;
- ensures the fusion of the virion membrane with the cell membrane and the membranes of its lysosomes, i.e. is responsible for the penetration of the virion into the cell;
- determines the pandemic nature of the virus (changes in hemagglutinin are the cause of pandemics, its variability is the cause of influenza epidemics);
- has the greatest protective properties, being responsible for the formation of immunity.
Influenza A viruses of humans, mammals and birds, 13 types of hemagglutinin, differing in antigen, have been identified and assigned a sequential numbering (from H1 to H13).
Neuraminidase (N) is a tetramer with a molecular weight of 200-250 kDa, each monomer has a molecular weight of 50-60 kDa. Its functions are:
- ensuring the dissemination of virions by cleaving neuraminic acid from newly synthesized virions and the cell membrane;
- together with hemagglutinin, determination of pandemic and epidemic properties of the virus.
Influenza A virus has been found to have 10 different neuraminidase variants (N1-N10).
The nucleocapsid of the virion consists of 8 fragments of vRNA and capsid proteins that form a helical strand. At the 3' ends of all 8 vRNA fragments there are identical sequences of 12 nucleotides. The 5' ends of each fragment also have identical sequences of 13 nucleotides. The 5' and 3' ends are partially complementary to each other. This circumstance obviously allows for the regulation of transcription and replication of the fragments. Each of the fragments is transcribed and replicated independently. Four capsid proteins are tightly associated with each of them: nucleoprotein (NP), which plays a structural and regulatory role; protein PB1 - transcriptase; PB2 - endonuclease and PA - replicase. Proteins PB1 and PB2 have basic (alkaline) properties, and PA - acidic. Proteins PB1, PB2 and PA form a polymer. The nucleocapsid is surrounded by a matrix protein (M1 protein), which plays a leading role in virion morphogenesis and protects virion RNA. Proteins M2 (encoded by one of the reading frames of the 7th fragment), NS1 and NS2 (encoded by the eighth fragment of vRNA, which, like the seventh fragment of vRNA, has two reading frames) are synthesized during virus reproduction, but are not included in its structure.
Life cycle of influenza A virus
The influenza virus is absorbed onto the cell membrane by the interaction of its hemagglutinin with the mucopeptide. The virus then enters the cell by one of two mechanisms:
- fusion of the virion membrane with the cell membrane or
- along the way: coated pit - coated vesicle - endosome - lysosome - fusion of the virion membrane with the lysosome membrane - release of the nucleocapsid into the cell cytosol.
The second stage of "undressing" the virion (destruction of the matrix protein) occurs on the way to the nucleus. The peculiarity of the life cycle of the influenza virus is that a primer is needed for the transcription of its vRNA. The fact is that the virus itself cannot synthesize a "cap" - a special region at the 5'-end of mRNA, consisting of methylated guanine and 10-13 adjacent nucleotides, which is necessary for the recognition of mRNA by the ribosome. Therefore, with the help of its protein PB2, it bites off the cap from the cellular mRNA, and since mRNA synthesis in cells occurs only in the nucleus, the viral RNA must first penetrate the nucleus. It penetrates it in the form of a ribonucleoprotein consisting of 8 RNA fragments associated with the proteins NP, PB1, PB2 and PA. Now the life of the cell is completely subordinated to the interests of the virus, its reproduction.
Transcription feature
In the nucleus, three types of virus-specific RNA are synthesized on vRNA: 1) positive complementary RNA (mRNA), used as templates for the synthesis of viral proteins; they contain a cap at the 5' end, cleaved from the 5' end of cellular mRNA, and a poly-A sequence at the 3' end; 2) full-length complementary RNA (cRNA), which serves as a template for the synthesis of virion RNA (vRNA); there is no cap at the 5' end of cRNA, and there is no poly-A sequence at the 3' end; 3) negative virion RNA (vRNA), which is the genome for newly synthesized virions.
Immediately, even before the completion of synthesis, vRNA and cRNA associate with capsid proteins, which enter the nucleus from the cytosol. However, only ribonucleoproteins associated with vRNA are included in the composition of virions. Ribonucleoproteins containing cRNA not only do not enter the composition of virions, but do not even leave the cell nucleus. Viral mRNAs enter the cytosol, where they are translated. Newly synthesized vRNA molecules migrate from the nucleus to the cytosol after association with capsid proteins.
 [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ]
[ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ]
Features of viral protein translation
Proteins NP, PB1, PB2, PA and M are synthesized on free polyribosomes. Proteins NP, PB1, PB2 and PA after synthesis from the cytosol return to the nucleus, where they bind to newly synthesized vRNA, and then return to the cytosol as a nucleocapsid. After synthesis, the matrix protein moves to the inner surface of the cell membrane, displacing cellular proteins from it in this area. Proteins H and N are synthesized on ribosomes associated with membranes of the endoplasmic reticulum, are transported along them, undergoing glycosylation, and are installed on the outer surface of the cell membrane, forming spikes just opposite protein M, located on its inner surface. Protein H undergoes cutting into HA1 and HA2 during processing.
The final stage of virion morphogenesis is controlled by the M protein. The nucleocapsid interacts with it; passing through the cell membrane, it is covered first by the M protein, and then by the cellular lipid layer and supercapsid glycoproteins H and N. The life cycle of the virus takes 6-8 hours and ends with the budding of newly synthesized virions, which are capable of attacking other cells of the tissue.
The virus is not very stable in the external environment. It is easily destroyed by heating (at 56 °C for 5-10 minutes), under the influence of sunlight and UV light, and is easily neutralized by disinfectants.
Pathogenesis and symptoms of influenza A
The incubation period for influenza is short - 1-2 days. The virus multiplies in the epithelial cells of the mucous membrane of the respiratory tract, primarily localizing in the trachea, which is clinically manifested as a dry, painful cough with pain along the trachea. The decay products of the affected cells enter the blood, causing severe intoxication and an increase in body temperature to 38-39 ° C. Increased vascular permeability due to damage to endothelial cells can cause pathological changes in various organs: pinpoint hemorrhages in the trachea, bronchi, and sometimes cerebral edema with a fatal outcome. The influenza virus has a depressing effect on hematopoiesis and the immune system. All this can lead to secondary viral and bacterial infections that complicate the course of the disease.
Post-infectious immunity
Previous ideas that after the flu there remains a weak and short-term immunity were refuted after the return of the H1N1 virus in 1977. This virus caused the disease mainly in people under 20 years of age, i.e. in those who had not been ill with it before 1957. Consequently, post-infection immunity is quite intense and long-lasting, but has a pronounced type-specific character.
The main role in the formation of acquired immunity belongs to virus-neutralizing antibodies that block hemagglutinin and neuraminidase, as well as secretory immunoglobulins IgAs.
Epidemiology of influenza A
The source of infection is a person, a sick person or a carrier, rarely animals (domestic and wild birds, pigs). Infection from people occurs through airborne droplets, the incubation period is very short (1-2 days), so the epidemic spreads very quickly and can develop into a pandemic in the absence of collective immunity. Immunity is the main regulator of influenza epidemics. As collective immunity increases, the epidemic declines. At the same time, due to the formation of immunity, strains of the virus with a modified antigenic structure are selected, primarily hemagglutinin and neuraminidase; these viruses continue to cause outbreaks until antibodies to them appear. Such antigenic drift maintains the continuity of the epidemic. However, another form of variability has been discovered in the influenza A virus, called shift. It is associated with a complete change from one type of hemagglutinin (less often - and neuraminidase) to another.
All flu pandemics were caused by influenza A viruses that had undergone a shift. The 1918 pandemic was caused by a virus with the H1N1 phenotype (about 20 million people died), the 1957 pandemic was caused by the h3N2 virus (more than half of the world's population fell ill), and the 1968 pandemic was caused by the H3N2 virus.
To explain the reasons for the sharp change in the types of influenza A viruses, two main hypotheses have been proposed. According to the hypothesis of A. A. Smorodintsev, a virus that has exhausted its epidemic capabilities does not disappear, but continues to circulate in a group without noticeable outbreaks or persists in the human body for a long time. In 10-20 years, when a new generation of people appears who do not have immunity to this virus, it becomes the cause of new epidemics. This hypothesis is supported by the fact that the influenza A virus with the H1N1 phenotype, which disappeared in 1957 when it was replaced by the h3N2 virus, reappeared after a 20-year absence in 1977.
According to another hypothesis, developed and supported by many authors, new types of influenza A virus arise as a result of reassociation of genomes between human and avian influenza viruses, between avian influenza viruses, between avian and mammalian (pig) influenza viruses, which is facilitated by the segmental structure of the viral genome (8 fragments).
Thus, the influenza A virus has two ways of changing its genome.
Point mutations causing antigenic drift. They primarily affect the hemagglutinin and neuraminidase genes, especially in the H3N2 virus. Due to this, the H3N2 virus caused 8 epidemics between 1982 and 1998 and remains of epidemic significance to this day.
Reassociation of genes between human influenza viruses and avian and swine influenza viruses. It is believed that the reassociation of the influenza A virus genomes with the avian and swine influenza virus genomes is the main reason for the emergence of pandemic variants of this virus. Antigenic drift allows the virus to overcome existing immunity in humans. Antigenic shift creates a new epidemic situation: most people have no immunity to the new virus, and a flu pandemic occurs. The possibility of such reassociation of the influenza A virus genomes has been proven experimentally.
It has been established that influenza epidemics in humans are caused by type A viruses of only 3 or 4 phenotypes: H1N1 (H0N1); h3N2; H3N2.
However, the chicken (bird) virus also poses a significant threat to humans. Outbreaks of chicken flu have been observed repeatedly, in particular, the chicken virus H5N1 caused a million-person epizootic among domestic and wild birds with 80-90% mortality. People have also become infected from chickens; in 1997, 18 people were infected from chickens, a third of whom died. A particularly large outbreak was observed in January-March 2004. It affected almost all the countries of Southeast Asia and one of the US states and caused enormous economic damage. 22 people were infected and died from chickens. The most rigorous and decisive measures were taken to eliminate this outbreak: strict quarantine, liquidation of all poultry in all foci, hospitalization and isolation of the sick and all people with elevated temperatures, as well as persons in contact with the sick, a ban on the import of chicken meat from the above-mentioned countries, strict medical and veterinary supervision of all passengers and vehicles arriving from these countries. The widespread spread of influenza among people did not occur because there was no reassociation of the genome of the bird flu virus with the genome of the human influenza virus. However, the danger of such reassociation remains real. This could lead to the emergence of a new dangerous pandemic human influenza virus.
The names of the detected strains of influenza viruses indicate the serotype of the virus (A, B, C), the host species (if it is not a human), the place of isolation, the strain number, the year of its isolation (the last 2 digits) and the phenotype (in parentheses). For example: "A/Singapore/1/57 (h3N2), A/duck/USSR/695/76 (H3N2)".
Laboratory diagnostics of influenza A
The material for the study is nasopharyngeal secretions, which are obtained either by washing or using cotton-gauze swabs, and blood. The following diagnostic methods are used:
- Virological - infection of chicken embryos, green monkey kidney cell cultures (Vero) and dogs (MDSC). Cell cultures are especially effective for isolating viruses A (H3N2) and B.
- Serological - detection of specific antibodies and an increase in their titer (in paired sera) using RTGA, RSK, and enzyme immunoassay.
- An immunofluorescence method is used as an accelerated diagnostic method, which allows for the rapid detection of viral antigen in smears from the nasal mucosa or in swabs from the nasopharynx of patients.
- For detection and identification of the virus (viral antigens), RNA probe and PCR methods have been proposed.
Treatment of influenza A
Treatment of influenza A, which should be started as early as possible, as well as prevention of influenza and other viral ARIs, is based on the use of dibazol, interferon and its inducers amixin and arbidol according to special regimens, and for the treatment and prevention of influenza in children over 1 year old - algirem (remantadine) according to special regimens.
Specific prevention of influenza A
Every year, hundreds of millions of people in the world get sick with flu, which causes enormous damage to the health of the population and the economy of each country. The only reliable means of combating it is the creation of collective immunity. The following types of vaccines have been proposed and used for this purpose:
- live from attenuated virus;
- killed whole virion;
- subvirion vaccine (from split virions);
- subunit - a vaccine containing only hemagglutinin and neuraminidase.
In our country, a trivalent polymer-subunit vaccine (“grippol”) has been created and is being used, in which a sterile conjugate of the surface proteins of viruses A and B is linked to the copolymer polyoxidonium (immunostimulant).
Children from 6 months to 12 years of age, according to WHO recommendations, should be vaccinated only with the subunit vaccine as the least reactogenic and toxic.
The main problem in increasing the effectiveness of influenza vaccines is to ensure their specificity against the current virus, i.e. the variant of the virus that caused the epidemic. In other words, the vaccine must contain specific antigens of the current virus. The main way to improve the quality of the vaccine is to use the most conservative epitopes common to all antigen variants of the virus A, which have maximum immunogenicity.

