
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Human granulocytic anaplasmosis
Medical expert of the article
Last reviewed: 12.07.2025
The infectious disease anaplasmosis is a transmissible pathology, that is, one that is transmitted by blood-sucking insects. In this case, the disease is spread by ixodid ticks, the same arthropods that can also transmit tick-borne encephalitis and borreliosis.
Anaplasmosis has polymorphic symptoms and characteristic seasonality (mainly spring-summer), associated with periods of natural tick activity. An infected person does not spread the infection, so contacts with him are not dangerous for others. [ 1 ]
Epidemiology
Anaplasmosis was first reported in 1994 by Chen et al. (J Clin Micro 1994; 32(3):589-595). Cases of anaplasmosis have been identified worldwide; in the United States, it is most commonly reported in the upper Midwest and Northeast. Disease activity has also been reported in northern Europe and Southeast Asia.[ 2 ],[ 3 ],[ 4 ],[ 5 ]
In Russia, anaplasma infection through ticks occurs in 5-20% (the overwhelming majority of cases occur in the Baikal region and Perm Krai). In Belarus, infection rates range from 4 to 25% (the highest prevalence is recorded in the forests of Belovezhskaya Pushcha). In Ukraine and Poland, the prevalence rate is approximately the same - 23%. The number of anaplasmosis cases in the United States reported to the CDC has steadily increased since the disease began to be recorded, from 348 cases in 2000 to a peak of 5,762 cases in 2017. Cases reported in 2018 were significantly lower, but increased to about 2017 in 2019 with 5,655 cases. [ 6 ]
Anaplasmosis is characterized by its seasonality, which corresponds to the active period of ixodid ticks. Spike in infections are observed from mid-spring to late summer, or more precisely, from April to early September. As a rule, anaplasmas are found in the same zonality as other types of infections transmitted by ticks, in particular, pathogenic borrelia. It has been determined that one ixodid tick can simultaneously carry up to seven pathogens of viral and microbial diseases. That is why more than half of cases of the disease are mixed infections - lesions by several infectious pathogens at the same time, which significantly worsens the outcome of the pathology. In most patients, anaplasmosis is detected in combination with tick-borne borreliosis or encephalitis, or with monocytic ehrlichiosis. In more than 80% of cases, co-infection with anaplasmosis and borreliosis is observed.
Causes anaplasmosis
The causative agent of the infectious pathology is anaplasma (full name Anaplasma phagocytophilum) - the smallest intracellular bacterium. When it enters the human bloodstream, it penetrates into granulocytes and spreads to all points of the body.
In natural conditions, anaplasma often settles in the bodies of mice and rats, and in inhabited areas dogs, cats, horses and other animals can become infected. However, they do not pose a danger to people: even if an infected animal bites a person, infection does not occur. [ 7 ]
The danger for people in terms of developing anaplasmosis is an attack by an ixodid tick, since during the bite it secretes saliva into the wound, which contains anaplasma.
The bacteria that causes anaplasmosis have diameters less than 1 micron. It enters the systemic bloodstream along with the insect's salivary fluid. When it gets into the tissue of internal organs, the pathogen activates the inflammatory process. The bacteria begin to multiply rapidly, which leads to suppression of the immune system and, as a consequence, the addition of secondary infectious diseases - microbial, viral or fungal.
The main reservoir is the white-footed mouse Peromyscus leucopus; however, a wide range of wild and domestic mammals have been identified as reservoirs. [ 8 ], [ 9 ] Ticks can spread the infection between wild and farm animals, particularly ungulates, dogs, rodents, and even birds that migrate regularly and thus facilitate wider transmission of the pathogen. Anaplasma lives in animals for several weeks, during which time previously uninfected insects become spreaders.
Risk factors
Blood-sucking ticks can carry various infections. The most well-known are tick-borne encephalitis and borreliosis, and such a pathogen as anaplasma was isolated only a few decades ago.
The risk of infection with anaplasma depends on the total number of ticks in a given area, the percentage of infected insects, and human behavior. In areas with a high risk of anaplasmosis, the danger primarily threatens those who rest or work in forest, forest plantation, and park areas - for example, special risk categories include hunters, fishermen, mushroom pickers, foresters, tourists, farmers, military personnel, etc.
Ixodid ticks are sensitive to climate: they choose to live in areas with moderate or abundant humidity, frequent precipitation, or covered by abundant thickets, where the humidity level can be maintained at around 80%. The insects' priority is deciduous and mixed forests, clearings, forest-steppe, parks, squares and gardens. Over the past few years, blood-sucking arthropods have spread quite widely to highland and northern regions. [ 10 ]
Pathogenesis
Anaplasmosis is transmitted when a tick attacks during bloodsucking. In the tick environment, the infection is transmitted from the female to the offspring, which causes constant circulation of pathogens. The contact route of transmission of anaplasma (through skin damage), as well as the digestive route (when consuming milk, meat) has not been proven.
People are most exposed to tick attacks in the spring and summer, when insect activity peaks. The start time of the tick season varies, depending on weather conditions. If the spring is warm and early, then the arthropods begin to "hunt" by the end of March, significantly increasing their activity by the second half of summer due to the accumulation of large volumes of bacteria.
Insects are active almost around the clock, but in warm sunny weather their highest aggressiveness is observed from eight to eleven o'clock in the morning, then gradually decreases and increases again from five to eight o'clock in the evening. In cloudy weather, the daily activity of ticks is approximately the same. Slowing down of activity is observed in hot conditions and during heavy rains.
Blood-sucking insects live mainly in massive, less often in small forests, forest belts and forest-steppes. Ticks are more common in damp places, in forest ravines, thickets, near streams and paths. They also live in cities: on the banks of rivers, in nature reserves, as well as parks and squares, and they sense the approach of a living object by smell from a distance of 10 meters.
The tick goes through several stages of development: egg, larva, nymph, adult. To ensure the normal course of all stages, the blood of a warm-blooded animal is required, so the tick diligently searches for a "breadwinner": it can be a small forest animal or bird, as well as large animals or livestock. In the process of sucking blood, the tick "shares" the bacteria with the animal, as a result of which it becomes an additional infection reservoir. A kind of bacterial circulation is obtained: from the tick to a living creature, and back to the tick again. In addition, bacterial cells can also spread from the insect to its offspring. [ 11 ]
Infection of people occurs in a transmissible way through tick bites. The pathogen enters the human body through bitten skin and penetrates the bloodstream, and then into various internal organs, including distant ones, which causes the clinical picture of anaplasmosis.
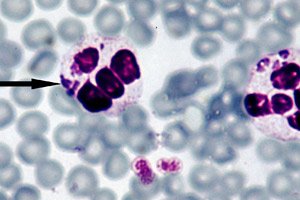
Anaplasma "infects" granulocytes, primarily mature neutrophils. Whole bacterial colonies of morula are formed inside the leukocyte cytosol. After infection, the pathogen penetrates the cell, begins to multiply in the vacuole of the cytoplasm and then leaves this cell. The pathological mechanism of the disease development is accompanied by damage to splenic macrophages, as well as liver and bone marrow cells, lymph nodes and other structures, inside which an inflammatory reaction begins to develop. Against the background of leukocyte damage and the development of the inflammatory process, the body's immune system is suppressed, which not only aggravates the situation, but also contributes to the emergence of a secondary infection of any origin. [ 12 ]
Symptoms anaplasmosis
With anaplasmosis, one can observe extensive symptoms of varying severity, which depends on the characteristics of the course of the disease. The first signs appear at the end of the latent incubation period, which lasts from several days to several weeks (usually about two weeks), if counted from the moment the bacteria enters the human bloodstream. [ 13 ]
In mild cases, the clinical picture is similar to a common ARVI - acute respiratory viral infection. The following symptoms are typical:
- a sharp deterioration in health;
- increase in temperature to 38.5°C;
- fever;
- a strong feeling of weakness;
- loss of appetite, dyspepsia;
- pain in the head, muscles, joints;
- sometimes – a feeling of pain and dryness in the throat, coughing, discomfort in the liver area.
In moderate cases, the severity of symptoms is more obvious. The following symptoms are added to the above:
- dizziness and other signs of neurology;
- frequent vomiting;
- difficulty breathing;
- decrease in daily diuresis (possible development of anuria);
- soft tissue swelling;
- slowing of the heartbeat, decrease in blood pressure;
- discomfort in the liver area.
If the patient suffers from immune deficiency, then against this background anaplasmosis is especially severe. The following symptoms are present:
- persistently elevated temperature, without normalization for several weeks;
- pronounced neurological signs, often with a picture of general brain damage (impaired consciousness - from lethargy to a comatose state), generalized seizures;
- increased bleeding, development of internal bleeding (blood in feces and urine, bloody vomiting);
- heart rhythm disturbances.
Manifestations of peripheral nervous system involvement include brachial plexopathy, cranial nerve palsies, demyelinating polyneuropathy, and bilateral facial nerve palsy. Recovery of neurological function may take several months.[ 14 ],[ 15 ],[ 16 ]
First signs
Immediately after the incubation period, which lasts on average 5-22 days, the first symptoms appear:
- sudden increase in temperature (febrile temperature);
- headache;
- severe fatigue, weakness;
- various manifestations of dyspepsia: from pain in the abdomen and liver area to severe vomiting;
- decreased blood pressure, dizziness;
- increased sweating.
Symptoms such as pain and burning in the throat, coughing are not found in all patients, but are not excluded. As you can see, the clinical picture is non-specific and rather resembles any viral respiratory infection, including influenza. Therefore, there is a high probability of making an erroneous diagnosis. Anaplasmosis can be suspected if the patient indicates a recent tick bite. [ 17 ]
Anaplasmosis in a child
If in adults anaplasmosis is transmitted by a tick bite, then in children there is another way of transmitting the infection - from mother to fetus. The disease is characterized by high temperature, headache and muscle pain, slow heartbeat and decreased blood pressure.
The clinical picture of anaplasmosis is most often represented by a moderate to severe form, however, such types of progression are characteristic mainly of adult patients. Children suffer from the infectious disease mainly in a mild form. Only in some cases, children develop anicteric hepatitis with increased transaminase activity. Even less often, kidney damage is observed with the development of hypoisosthenuria, proteinuria and erythrocyturia, as well as an increase in the level of creatinine and urea in the blood. In isolated cases, the pathology is complicated by infectious toxic shock, acute renal failure, acute respiratory distress syndrome, meningoencephalitis. [ 18 ]
Treatment of the disease in childhood, as well as in adults, is based on taking Doxycycline. It is generally accepted that this drug is prescribed to children from the age of 12. However, there were cases of earlier treatment with Doxycycline - in particular, from the age of 3-4. The dosage is selected individually.
Stages
There are three stages of development of anaplasmosis: acute, subclinical and chronic.
The acute stage is characterized by temperature fluctuations to high values (40-41°C), sharp weight loss and weakness, dyspnea-type shortness of breath, enlarged lymph nodes, the appearance of purulent rhinitis and conjunctivitis, and an enlarged spleen. Some patients experience increased sensitivity caused by irritation of the meninges, as well as seizures, muscle twitching, polyarthritis, and cranial nerve paralysis. [ 19 ]
The acute stage gradually transforms into a subclinical stage, in which anemia, thrombocytopenia, leukopenia (in some cases, leukocytosis) are observed. Then, after about 1.5 to 4 months (even in the absence of treatment), either recovery or the next, chronic stage of the disease may occur. It is characterized by anemia, thrombocytopenia, edema, and the addition of secondary infectious pathologies. [ 20 ]
Forms
Depending on the intensity of symptoms, the following types of anaplasmosis are distinguished:
- latent, asymptomatic (subclinical);
- manifest (explicit).
Depending on the severity of the infectious disease, mild, moderate and severe cases are distinguished.
In addition, a distinction is made between platelet and granulocytic anaplasmosis, however, platelet damage is characteristic only in relation to veterinary medicine, as it is found mainly in cats and dogs. [ 21 ]
Anaplasma is a pathogen not only in humans, but also in dogs, cows, horses and other species of animals. Tick-borne anaplasmosis in humans can be found almost anywhere in the world, since the carriers of the disease - ticks - live in both European and Asian countries.
Anaplasmosis of cattle and other farm animals is a long-known disease, which was first described in the 18th century: it was then called tick fever, it affected mainly goats, calves and sheep. The existence of granulocytic anaplasmosis in horses was officially confirmed in 1969, and in dogs - in 1982. [ 22 ] In addition to ticks, horseflies, stinging flies, midges, sheep bloodsuckers, and black flies can become carriers of the infection.
Anaplasmosis in sheep and other farm animals is manifested by the following initial signs:
- sudden increase in temperature;
- yellowing of the mucous tissues due to excess bilirubin in the bloodstream;
- difficulty breathing, heavy breathing, signs of hypoxia;
- rapid heartbeat;
- rapid weight loss;
- loss of appetite;
- apathy, lethargy;
- digestive disorders;
- decrease in milk yield;
- edema (dewlap and limbs);
- coughing.
Animal infection is often determined by eating disorders. Thus, sick individuals, due to impaired metabolism, try to taste and chew inedible objects. Metabolic failure, suppression of oxidation-reduction processes lead to disruption of hematopoiesis, a drop in the level of hemoglobin in the blood, and the development of hypoxia. Intoxication entails the development of inflammatory reactions, edema and hemorrhage are observed. The correct diagnosis and timely prescription of treatment play a decisive role in the prognosis of pathology. [ 23 ]
A considerable number of not only domestic but also wild animals can act as a reservoir for the causative agent of anaplasmosis. At the same time, dogs, cats, and even humans themselves are accidental hosts that do not play the role of a transmitter of infection to other living beings.
Anaplasmosis in cats is the rarest – only in isolated cases. Animals become easily tired, tend to avoid any activity, mostly rest, and practically do not eat. Jaundice often develops.
Anaplasmosis in dogs also does not have specific symptoms. Depression, fever, enlarged liver and spleen, lameness are noted. There are descriptions of coughing, vomiting and diarrhea in animals. It is noteworthy that in North America the pathology has a predominantly mild course, while in European countries fatal outcomes are often observed.
For most animals, the prognosis for anaplasmosis is favorable, provided that antibiotic therapy is administered in a timely manner. The blood picture stabilizes within 2 weeks from the start of therapy. Fatal outcomes among dogs and cats have not been described. A more complex course of the pathology is observed with a combined infection, when anaplasma is combined with other pathogens transmitted during a tick bite. [ 24 ]
Complications and consequences
If a patient with anaplasmosis does not seek medical attention, or the treatment is initially prescribed incorrectly, the risk of complications increases significantly. Unfortunately, this happens quite often, and instead of a rickettsial infection, the patient begins to be treated for acute respiratory viral infection, influenza, or acute bronchitis. [ 25 ]
It is important to understand that complications of an infectious disease can really be dangerous, as they often lead to serious consequences, and even death of the patient. Among the most common complications are the following:
- monoinfection;
- renal failure;
- central nervous system damage;
- cardiac failure, myocarditis;
- pulmonary aspergillosis, respiratory failure;
- infectious toxic shock;
- atypical pneumonia;
- coagulopathy, internal bleeding;
- meningoencephalitis.
These are the most common, but not all known consequences that can develop as a result of anaplasmosis. Of course, there are cases of spontaneous recovery of the disease, which is typical for people with good and strong immunity. However, if the immune defense is impaired - for example, if a person has recently been ill or suffers from chronic diseases, or has taken immunosuppressant therapy, or has had surgery, then the development of complications in such a patient is more than likely. [ 26 ]
The most unfavorable outcome may be the death of the patient as a result of multiple organ failure.
Diagnostics anaplasmosis
An important role in diagnosing anaplasmosis is played by collecting epidemiological anamnesis. The doctor must pay attention to such moments as tick bites, the patient's stay in an infectious endemic region, his visits to forests and forest parks over the past month. The obtained epidemiological information in combination with the existing symptoms helps to get oriented and conduct diagnostics in the right direction. Changes in the blood picture provide additional assistance, but the main diagnostic moment is a laboratory study.
The most effective way to diagnose anaplasmosis is considered to be direct dark-field microscopy, the essence of which is the visualization of embryonic structures - morulae - inside neutrophils, during light microscopy of a thin blood smear stained with Romanovsky-Giemsa. A visible morula is formed approximately from the third to the seventh day after the introduction of the bacteria. A relatively simple research method also has a certain disadvantage, since it shows insufficient efficiency at low levels of anaplasma in the blood. [ 27 ]
General clinical examinations and, in particular, a complete blood count demonstrate leukopenia with a left shift in the leukocyte formula, a moderate increase in ESR. Many patients have anemia and pancytopenia.
General urine analysis reveals hypoisosthenuria, hematuria, and proteinuria.
Blood biochemistry indicates increased activity of liver tests (AST, ALT), LDH, increased levels of urea, creatinine and C-reactive protein.
Antibodies to anaplasmosis are determined by the serological reaction method (ELISA). Diagnostics is based on determining the dynamics of titers of specific antibodies to bacterial antigens. Initial IgM antibodies appear from the eleventh day of the disease, reaching a peak amount from the 12th to the 17th day. Then their number decreases. IgG antibodies can be detected already on the first day of the infectious process: their concentration gradually increases, and the peak level occurs at 37-39 days. [ 28 ]
PCR for anaplasmosis is the second most common direct diagnostic method that detects anaplasma DNA. The biomaterial for PCR analysis is blood plasma, leukocyte fraction, cerebrospinal fluid. It is also possible to examine the tick, if there is one.
Instrumental diagnostics involves the following procedures:
- X-ray examination of the lungs (picture of bronchitis or pneumonia, enlarged lymph nodes);
- electrocardiography (picture of impaired conduction);
- ultrasound examination of abdominal organs (enlarged liver, diffusely altered liver tissue).
Differential diagnosis
Differentiation of various endemic rickettsial diseases is performed taking into account clinical and epidemiological signs. It is important to pay attention to epidemiological data typical for most endemic rickettsioses (travel to an endemic focus, seasonality, tick attacks, etc.), as well as to such symptoms as the absence of primary affect, regional enlargement of lymph nodes, and the absence of a rash.
In some cases, anaplasmosis may resemble epidemic typhus with a moderate course, as well as a mild form of Bril's disease. In typhus, neurological symptoms are more pronounced, roseolous-petechial rash is present, there are Chiari-Avtsyn and Govorov-Godelier symptoms, tachycardia, Rosenberg enanthem, etc. [ 29 ]
It is important to distinguish anaplasmosis from flu and ARVI in a timely manner. With flu, the febrile period is short (3-4 days), headache is concentrated in the superciliary and temporal region. Catarrhal symptoms are present (coughing, runny nose), there is no enlargement of the liver.
Another disease that requires differentiation is leptospirosis. The pathology is characterized by severe pain in the calf muscles, scleritis, rapid heartbeat, neutrophilic leukocytosis. Severe leptospirosis is characterized by jaundice of the sclera and skin, meningeal syndrome, cerebrospinal fluid changes of the serous meningitis type. The diagnosis is established by determining leptospira in the bloodstream and urine, as well as a positive agglutination and lysis reaction.
Dengue fever is characterized by a two-wave temperature curve, severe joint pain, typical changes in gait, and initial tachycardia. With the second wave, an itchy rash appears, followed by peeling. Diagnosis is based on the isolation of the virus.
Brucellosis is characterized by undulating fever, profuse sweating, migrating arthralgia and myalgia, micropolyadenitis with subsequent damage to the musculoskeletal system, nervous and genitourinary system. [ 30 ]
Ehrlichiosis and anaplasmosis are two rickettsial infections that have many similarities in their clinical course. The diseases often begin acutely, like an acute viral infection. Non-specific symptoms include a strong increase in temperature with chills, weakness, muscle pain, nausea and vomiting, coughing, and headache. However, skin rashes are not typical for anaplasmosis, unlike ehrlichiosis, which is characterized by papular or petechial elements on the extremities and trunk.
Both anaplasmosis and ehrlichiosis can be complicated by disseminated intravascular coagulation, multiple organ failure, convulsive syndrome, and development of a comatose state. Both diseases are classified as infections with a complex course associated with an increased risk of death in people with immunodeficiency. The development of an infectious process is especially dangerous in patients who have previously taken immunosuppressant treatment, have undergone surgery to remove the spleen, or in HIV-infected patients.
Serological tests and PCR play the main differential role in diagnosing anaplasmosis or ehrlichiosis. Cytoplasmic inclusions are detected in monocytes (in ehrlichiosis) or granulocytes (in anaplasmosis).
Borreliosis and anaplasmosis have a common endemic prevalence, develop after a bite of an ixodid tick, but the clinical picture of these infections is different. With borreliosis, a local skin inflammatory reaction is observed at the site of the bite, called tick-borne erythema migrans, although an erythematous course of the disease is also possible. As borrelia spreads throughout the body, the musculoskeletal system, nervous and cardiovascular systems, and skin are affected. Lameness, lethargy, and cardiac dysfunction are characteristic. About six months after infection, severe joint damage occurs, and the nervous system suffers. Diagnostics is reduced to the use of ELISA, PCR, and immunoblotting methods. [ 31 ]
Who to contact?
Treatment anaplasmosis
The main treatment for anaplasmosis is antibiotic therapy. The bacteria are sensitive to tetracycline antibacterial drugs, so the choice often falls on Doxycycline, which patients take orally at 100 mg twice a day. The duration of treatment is from 10 days to three weeks. [ 32 ]
In addition to tetracycline drugs, anaplasma is also sensitive to amphenicols, in particular, to Levomycetin. However, the use of this antibiotic is not encouraged by specialists, which is associated with the pronounced side effects of the drug: during treatment, patients develop granulocytopenia, leukopenia, thrombocytopenia. [ 33 ]
Female patients during pregnancy and lactation are prescribed Amoxicillin or protected penicillins in individual dosages.
If antibiotics are prescribed within three days after the tick bite, then a shortened course of therapy is carried out - for a week. If you contact a doctor later, the full treatment regimen is used.
Additionally, symptomatic therapy is carried out, during which the following groups of drugs may be prescribed:
- nonsteroidal anti-inflammatory drugs;
- hepatoprotectors;
- multivitamin products;
- antipyretics;
- painkillers;
- medications for the correction of concomitant disorders of the respiratory, cardiovascular, and nervous systems.
The clinical effectiveness of the therapy is assessed based on its results: positive signs include a decrease in the severity and disappearance of symptoms, normalizing dynamics of disorders in laboratory and instrumental studies, and changes in the titers of specific antibodies to anaplasma. If necessary, the drugs are replaced and a repeated course of treatment is prescribed.
Medicines
The most commonly used treatment regimen for anaplasmosis is:
- Doxycycline or its soluble analogue Unidox Solutab – 100 mg twice a day;
- Amoxicillin (as indicated, or if it is impossible to use Doxycycline) – 500 mg three times a day;
- In severe cases of anaplasmosis, the optimal drug is considered to be Ceftriaxone in the amount of 2 g intravenously once a day.
Penicillin preparations, second- and third-generation cephalosporins, and macrolides can also be considered as alternative antibiotics.
Since the use of antibiotics for anaplasmosis is usually long-term, the consequences of such therapy can be very different: most often, side effects are expressed in digestive disorders, skin rashes. After completion of the treatment course, a set of measures is necessarily prescribed to eliminate such consequences and restore adequate functioning of the digestive system.
The most common consequence of antibiotic therapy is intestinal dysbacteriosis, which develops as a result of the depressing effect of antibacterial drugs on both pathogenic microorganisms and the natural microflora in the body. To restore such microflora, the doctor prescribes probiotics and eubiotics.
In addition to dysbacteriosis, prolonged antibiotic therapy can contribute to the development of fungal infections. For example, oral and vaginal candidiasis often develops.
Another possible side effect is allergy, which can be limited (rash, rhinitis) or complex (anaphylactic shock, Quincke's edema). Such conditions require immediate discontinuation (replacement) of the drug and emergency antiallergic measures, using antihistamines and glucocorticoids.
Along with antibiotic therapy, symptomatic drugs are prescribed. Thus, in case of elevated temperature, severe intoxication, detoxifying solutions are used, in case of edema - dehydration, in case of neuritis, arthritis and joint pain - non-steroidal anti-inflammatory drugs and physiotherapy. Patients with a picture of cardiovascular damage are prescribed Asparkam or Panangin 500 mg three times a day, Riboxin 200 mg 4 times a day.
If an immunodeficiency condition is detected, Timalin is indicated at 10-30 mg daily for two weeks. For patients with autoimmune manifestations - for example, with recurrent arthritis - Delagil is recommended at 250 mg daily in combination with non-steroidal anti-inflammatory drugs.
Vitamin therapy involves the use of drugs containing vitamins C and E.
Additionally, vascular agents (Nicotinic acid, Complamin) are included in the treatment regimen. To facilitate the penetration of antibacterial drugs into the central nervous system, patients are given Euphyllin, glucose solution, as well as drugs to optimize cerebral circulation and nootropics (Piracetam, Cinnarizine).
In chronic cases of the disease, immunocorrective treatment is indicated.
Prevention
Anaplasmosis carriers live on the ground, but can climb tall grass and bushes up to 0.7 m high and wait there for a potential carrier. A tick attack is practically not felt by a person, so people often do not pay attention to the bite.
For preventive purposes, it is recommended to wear clothes that can protect against insect attacks, and if necessary, use special repellents. After each walk (especially in the forest), you should check your entire body: if a tick is found, it must be removed immediately. The removal procedure is carried out using tweezers or pointed tongs, grasping the arthropod as close as possible to the area of adjacent to the skin surface. It must be pulled out very carefully, with shaking and twisting movements, trying to ensure that parts of the tick's body do not come off and do not remain in the wound. To prevent infection, it is important to treat the bitten area with an antiseptic at the end of the procedure.
After any, even a short stay in the forest belt, it is necessary to check the skin, and not only in visible places: it is imperative to check the skin folds, since insects often strive for areas with high humidity on the body - for example, in the armpits and groin, under the mammary glands, on the folds of the arms and legs. In children, among other things, it is important to carefully examine the head and neck, the area behind the ears. [ 34 ]
Before entering the apartment, it is advisable to also inspect things and clothes, because insects can be brought in even in a bag or on shoes.
To prevent infection with anaplasmosis, it is recommended:
- avoid walking in places where blood-sucking insects may live;
- have an understanding of how to properly remove ticks and the first signs of anaplasmosis infection;
- If necessary, be sure to use insect repellents;
- For forest and park walks, wear appropriate clothing (long sleeves, covered ankles and feet).
Forecast
For the overwhelming majority of patients with anaplasmosis, the prognosis is assessed as positive. As a rule, about 50% of patients require inpatient treatment. In some infected people, the disease is cured on its own, but some painful symptoms disappear only after some time - within a few months.
A worsening of the prognosis is observed with the development of hematological and neurological complications, which is typical for patients with immunodeficiency states, chronic liver and kidney diseases. Mortality is relatively low. [ 35 ]
In general, the course and outcome of the pathology depend on the correct diagnosis, timely administration of antibacterial and symptomatic drugs. In moderate and severe cases, patients are placed in an infectious diseases hospital. It is important to provide the patient with rest, good hygiene and nutrition. During periods of increased temperature and fever, the patient's diet should be extremely gentle, both mechanically and chemically and thermally, minimizing products that cause fermentation and putrefaction in the intestines. At the same time, meals should be high in calories. Bed rest should be observed until the temperature returns to normal, plus a few more days. It is important to use effective etiotropic agents that increase the specific and non-specific reactivity of the body.
If the patient was treated late or treated incorrectly, the disease may become chronic. People who have had anaplasmosis are subject to medical observation of the dynamics for 12 months. Observation involves regular examination by an infectious disease specialist, a therapist, and, if necessary, a neurologist. [ 36 ]
Cattle that have had anaplasmosis become temporarily immune to the infection. But this immunity does not last long: about four months. If a pregnant female has had the disease, her offspring will have longer immunity to the infection due to the presence of antibodies in the blood. If the offspring does become infected, the disease will be milder.

