
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Fibrous osteodysplasia.
Medical expert of the article
Last reviewed: 04.07.2025
Bone dysplasia, Lichtenstein-Braitzev disease, fibrous osteodysplasia - all these are the names of the same congenital non-hereditary pathology, in which bone tissue is replaced by fibrous tissue. Patients have bone curvatures - mainly in childhood and adolescence. Almost any of the skeletal bones can be damaged, but the most frequently affected are the bones of the skull, ribs and long tubular bones (metaphyseal and diaphyseal parts, without involving the epiphysis). Multiple lesions are often combined with McCune-Albright syndrome. Clinical symptoms depend on which bones are affected and to what extent. Treatment is mainly surgical.
Epidemiology
Cases of fibrous osteodysplasia account for approximately 5% of all benign bone pathologies. However, there is no clear data on the true incidence rate, since the disease is often asymptomatic (in approximately 40% of cases, patients do not present any complaints). At the same time, localized fibrous osteodysplasia is reported in approximately 78% of cases.
The course of fibrous osteodysplasia is slow, progressive, and manifests itself mainly during periods of increased bone growth. That is why the pathology is most often detected in adolescents aged 13-15 (30% of examined patients). However, it happens that the problem is first detected in old age. If the disease simultaneously affects several bones (and this happens in approximately 23% of cases), the anomaly can be detected much earlier – in patients of preschool and school age.
Almost half of patients, along with fibrous osteodysplasia, also have other diseases of the musculoskeletal system.
Not all patients have obvious symptoms of the disease. The risk of pathology increases during puberty, in women - during pregnancy, and also when exposed to harmful external and internal factors.
Representatives of the female and male sexes are equally affected (according to other data, girls are affected somewhat more often, in a ratio of 1:1.4).
The most frequently observed lesions are those of the femur (47%), shin bones (37%), shoulder bones (12%) and forearm (2%). Fibrous osteodysplasia can occur with equal frequency on both the left and right sides. The polyostotic type of pathology often spreads to the bones of the skull, pelvis and ribs (25% of cases).
Causes fibrous osteodysplasia
Fibrous osteodysplasia is a systemic pathology of skeletal bones, congenital but not hereditary. Dysplasia processes resemble tumor formation, while not being a real tumor process. Pathology appears as a result of disruption of the development of the bone tissue progenitor - skeletogenic mesenchyme.
The first description of fibrous osteodysplasia was made at the beginning of the 20th century by the Russian doctor Braitsov. Subsequently, information about the disease was supplemented by the American endocrinologist Albright, the orthopedist Albrecht and other specialists (in particular, Lichtenstein and Jaffe).
In medicine, the following types of pathology are distinguished:
- monostotic (when one bone of the skeleton is affected);
- polyostotic (when two or more bones of the skeleton are affected).
The first pathological type can first appear at almost any age and is usually not accompanied by hyperpigmentation or disruption of the endocrine system.
The second pathological type is found in pediatric patients and usually occurs as Albright syndrome.
Most often, specialists use the following clinical and pathological classification of fibrous osteodysplasia:
- Intraosseous lesion, with the formation of single or multiple fibrous foci inside the bone. Less often, the entire bone is affected, with structural preservation of the cortex and the absence of curvature.
- Total osteodysplasia, with involvement of all segments in the process, including the cortical layer and the bone marrow cavity zone. The lesion is accompanied by bone curvature, pathological fractures. Long tubular bones are predominantly damaged.
- The tumor lesion is characterized by focal spread of fibrosis. Such growths are often distinguished by their pronounced size.
- Albright syndrome is characterized by multiple bone pathologies against the background of endocrine disorders, early onset of puberty, abnormal body proportions, skin hyperpigmentation and pronounced bone curvatures.
- Fibrocartilaginous lesions are accompanied by transformation of cartilaginous tissue, which is often complicated by the development of chondrosarcoma.
- Calcifying lesion is characteristic of fibrous osteodysplasia of the tibia.
Risk factors
Since fibrous osteodysplasia is not a hereditary disease, intrauterine disturbances in the formation of tissues from which the skeletal system subsequently develops are considered as causative factors.
It is possible that the causes may be various pregnancy pathologies, in particular, vitamin deficiency, endocrine disorders, as well as environmental factors such as radiation and infectious effects.
In general, risk factors are described as follows:
- toxicosis in a woman in the first half of pregnancy;
- viral and microbial infections in women up to 15 weeks of pregnancy;
- unfavorable environmental conditions;
- vitamin deficiency (vitamins B and E), as well as lack of iron, calcium, iodine.
Pathogenesis
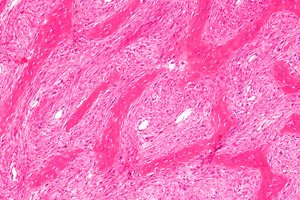
The development of fibrous osteodysplasia is caused by a change in the DNA sequence of somatic cells in the GNAS1 gene, located on chromosome 20q13.2-13.3. This gene is responsible for encoding the α-subunit of the activating protein G. As a result of mutational changes, the amino acid arginine R201 is replaced by the amino acid cysteine R201C or histidine R201H. Under the influence of the abnormal type of protein, activation of G1 cyclic AMP (adenosine monophosphate) occurs and osteoblastic cells accelerate DNA production, different from the norm. As a result, fibrous disorganized bone matrix tissue and primitive bone tissue are formed, deprived of the property of maturation into a lamellar structure. Pathological changes also affect mineralizing processes. [ 1 ]
Skeletal stem cells that carry this mutation have an impaired ability to differentiate into mature osteoblasts and instead retain a fibroblast-like phenotype.[ 2 ],[ 3 ] The mutant cells proliferate and replace normal bone and bone marrow, typically with demineralized and structurally immature fibro-osseous tissue.[ 4 ],[ 5 ]
Basic pathogenetic characteristics of fibrous osteodysplasia development also include formation and growth of cysts due to local disorder of venous outflow in bone metaphysis. Pathological process leads to increase of intraosseous pressure, change of cellular composition of blood, release of lysosome enzymes affecting bone tissue and provoking its lysis. At the same time, coagulation process is disrupted, local fibrinolysis is observed. Accumulation of bone matrix decomposition products causes increase of oncotic pressure inside cystic formation. Pathological cycle of mutual amplification of disorders is formed.
Symptoms fibrous osteodysplasia
Fibrous osteodysplasia most often manifests itself in early childhood and adolescence. The humerus, ulna, radius, femur, tibia, and fibula are predominantly affected.
The initial stage of the disease is not accompanied by any pronounced symptoms, sometimes slight nagging pains are noted. [ 6 ], [ 7 ] In many patients, the first "alarm bell" is a pathological fracture. In general, the first signs are often absent or remain unnoticed.
When palpated, there is usually no pain: pain is more typical for significant physical exertion. If the pathological process affects the proximal femoral diaphysis, the patient may experience lameness, and in case of pathology of the humeral bone, the patient may note discomfort during a sharp swing and lifting of the limb. [ 8 ], [ 9 ]
The clinical picture of fibrous osteodysplasia is not always detected in children, since many patients most often do not have congenital anomalies and curvatures. But the polyostotic type of pathology manifests itself precisely in young children. Bone disorders are combined with endocrinopathy, skin hyperpigmentation, and cardiovascular disorders. The symptoms of the disease can be varied and multifaceted. In this case, the main symptom is pain syndrome against the background of increasing deformation.
Many patients are diagnosed with fibrous dysplasia after a pathological fracture is discovered.
The severity of bone curvatures depends on the location of the pathological lesion. If the tubular bones of the hands are affected, their club-shaped enlargement is possible. If the finger phalanges are affected, their shortening, "chopping off", is observed.
Complications and consequences
The most common consequences of fibrous osteodysplasia are pain and increasing deformities of individual bones and limbs, as well as pathological fractures.
The leg bones are often deformed due to the pressure of body weight, typical curvatures appear. The most pronounced curvature is the femur, which in some cases shortens by several centimeters. When the femoral neck is deformed, a person begins to limp.
With fibrous osteodysplasia of the ischium and ilium, the pelvic ring is curved, which causes corresponding complications on the part of the spinal column. Kyphosis or kyphoscoliosis is formed. [ 10 ]
Monostotic dysplasia is considered to have a more favorable prognosis, although the risk of pathological fractures is present.
Malignant degeneration of fibrous osteodysplasia is rare, but it should not be completely excluded. The development of such tumor processes as osteosarcoma, fibrosarcoma, chondrosarcoma, malignant fibrous histiocytoma is possible.
Diagnostics fibrous osteodysplasia
The diagnosis is made by an orthopedic specialist based on the characteristics of clinical manifestations and information obtained during instrumental and laboratory diagnostics.
The traumatological and orthopedic status is studied without fail, the sizes of the affected and healthy limbs are measured, the amplitude of joint movements (active and passive) and the condition of soft tissue structures are assessed, and curvature indicators and cicatricial changes are determined.
An examination by an orthopedist consists of the following stages:
- external examination of the affected area, detection of redness, swelling, muscle atrophy, damage to the skin, ulcerative processes, curvatures, shortening of the bone;
- palpation of the affected area, detection of compactions, tissue softening, fluctuating elements, palpation pain, excessive mobility;
- taking measurements, detecting hidden edema, muscle atrophy, changes in bone length;
- volumetric measurements of joint movements, detection of joint diseases.
Thanks to the external examination, the doctor can suspect a particular disease or injury, note its localization and prevalence, describe pathological signs. After this, the patient is assigned laboratory tests.
The tests may include clinical and biochemical blood tests, a coagulogram, urine analysis, and an assessment of the immune status. The white blood cell count, total protein, albumin, urea, creatinine, alanine aminotransferase, and aspartate aminotransferase levels are determined, the electrolytic composition of the blood is examined, and histology of biopsies and punctures is performed. If indicated, genetic tests are prescribed.
Instrumental diagnostics are necessarily represented by radiography (lateral and direct). Sometimes, to determine the characteristics of the deformation, oblique projections with a rotation angle of 30 to 40 degrees are additionally prescribed.
In many cases, a CT scan of the damaged bone is recommended. This allows for a more precise determination of the location and size of the defects.
Magnetic resonance imaging helps to assess the condition of surrounding tissues, and ultrasound examination of the extremities determines vascular disorders.
The radionuclide technique – two-phase scintigraphy – is necessary to identify affected areas that are not visualized by conventional radiography, as well as to assess the scope of the operation.
X-ray is considered a mandatory diagnostic method for patients with suspected fibrous osteodysplasia, as it helps to identify the stage of the pathology. For example, at the osteolysis stage, the image shows a structureless, sparse metaphysis touching the growth zone. At the demarcation stage, the image shows a cellular cavity with a dense-walled environment, separated from the growth zone by a part of healthy bone tissue. At the recovery stage, the image reveals an area of compacted bone tissue or a small residual cavity. In patients with fibrous osteodysplasia, the normal metaphyseal image is replaced by a zone of enlightenment: such a zone is localized longitudinally, sharpens towards the bone center and expands towards the growth disc. It is characterized by unevenness, fan-shaped shading by bone partitions towards the epiphyses.
X-rays are always taken in different projections, which is necessary to clarify the distribution of fibrous areas.
A non-specific radiographic sign is the periosteal reaction, or periostitis (periostosis). The periosteal reaction in fibrous osteodysplasia is a response of the periosteum to the effect of an irritating factor. The periosteum is not detected on an X-ray image: the reaction occurs only in the case of ossification of the periosteal layers.
Differential diagnosis
Differential diagnostics of bone and joint diseases is multifaceted and quite complex. According to clinical and diagnostic recommendations, it is advisable to use a multiple approach, using information obtained as a result of radiography, computed tomography, magnetic resonance imaging, ultrasound examination. If possible, all available methods of radiation diagnostics should be used:
- polypositional, comparative radiography;
- bone mode in computed tomography, etc.
Fibrous osteodysplasia should be distinguished from the following pathologies:
- osteofibrous dysplasia (ossifying fibroma);
- parosteal osteosarcoma;
- giant cell reparative bone granuloma;
- Paget's disease;
- well-differentiated central osteosarcoma. [ 11 ]
Who to contact?
Treatment fibrous osteodysplasia
Drug therapy for patients with fibrous osteodysplasia is practically ineffective. Relapses of the disease are quite common, as well as increasing dynamics of curvature and changes in bone length. [ 12 ]
A positive effect of puncture therapy in the development of cystic formations has been noted, but such treatment does not solve the general problem, which is associated with pronounced deformations and changes in bone length.
Thus, the only sure way to stop fibrous osteodysplasia is considered to be surgical intervention, which is recommended for patients with tubular bone dysplasia with background deformities.
In the absence of deformation of the bone diaphysis and the presence of 50-70% damage to the bone cross-section, intrafocal resection is performed. The intervention is performed taking into account the information obtained during computed tomography and radioisotope diagnostics. The defect is replaced with longitudinally split cortical grafts. In case of severe damage to the bone cross-section (more than 75%), it is recommended to perform an operation to radically remove the altered tissue. [ 13 ] The defect is replaced with cortical grafts, simultaneously using different types of osteosynthesis:
- metal osteosynthesis using extra-osseous fixation devices is recommended for patients with femoral deformities and the transition of the pathological process to the trochanteric region and segmental neck;
- Metal osteosynthesis using straight periosteal plates is recommended for patients with tibial curvature.
Osteosynthesis surgery is planned and may have its own contraindications:
- acute course of infectious and inflammatory pathologies;
- exacerbation of chronic pathologies;
- states of decompensation;
- psychopathologies;
- dermatopathologies affecting the area affected by fibrous osteodysplasia.
The essence of the surgical intervention is a complete segmental resection of damaged bone tissue and installation of a bone implant. In the presence of a pathological fracture, the Ilizarov transosseous compression-distraction apparatus is used.
In case of polyostotic damage, it is recommended to start surgical intervention as early as possible, without waiting for the appearance of curvatures of the damaged bones. In this situation, we can talk about a preventive (warning) operation, which is technically easier, and also has a softer rehabilitation period.
Cortical grafts can resist dysplasia for a long period of time, and together with bone fixation devices help prevent re-deformation of the operated limb and prevent the occurrence of a pathological fracture.
Patients with fibrous osteodysplasia who have undergone surgery require systematic dynamic monitoring by an orthopedic surgeon, since the disease has a tendency to relapse. If osteodysplasia relapses, a second operation is usually prescribed. [ 14 ]
The postoperative recovery period is long. It includes exercise therapy to prevent contractures, as well as spa treatment.
Prevention
There is no specific prevention for the development of fibrous dysplasia, which is due to the poorly understood etiology of the disorder.
Preventive measures include adequate pregnancy management and following the following recommendations:
- optimization of a woman’s nutrition throughout the entire reproductive period, ensuring the necessary intake of microelements and vitamins;
- elimination of alcohol consumption and smoking;
- prevention of the negative impact of teratogenic substances (heavy metal salts, insecticides, pesticides and some medications);
- improving women’s somatic health (maintaining normal body weight, preventing diabetes, etc.);
- prevention of development of intrauterine infections.
After the birth of a child, it is important to think in advance about the prevention of both fibrous osteodysplasia and pathologies of the musculoskeletal mechanism in general. Doctors suggest using the following recommendations:
- watch your weight;
- be physically active and at the same time not overload the musculoskeletal system;
- avoid constant excessive stress on bones and joints;
- ensure adequate supply of vitamins and minerals to the body;
- give up smoking and alcohol abuse.
In addition, it is necessary to promptly seek medical help for injuries and pathologies of the musculoskeletal system. Trauma management should be complete, and you should not complete treatment on your own without consulting a doctor. It is important to undergo regular medical examinations - especially if a person is at risk or experiences discomfort in the bones, joints, or spine.
Forecast
The prognosis for life of patients with fibrous osteodysplasia is favorable. However, in the absence of treatment or with inappropriate therapeutic measures (especially in case of polyostotic lesions), there is a risk of developing gross curvatures leading to disability. In some patients, fibrous osteodysplasia leads to the fact that dysplastic foci are transformed into benign and malignant tumor processes - thus, there were fixed cases of the development of giant cell neoplasm, osteogenic sarcoma, non-ossifying fibroma.
Fibrous osteodysplasia has a tendency to frequent relapses. Therefore, it is very important that the patient, even after the surgical intervention, is under constant observation of orthopedic specialists. Formation of new pathological foci, lysis of allografts, pathological fractures are not excluded.

