
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Fibroelastosis
Medical expert of the article
Last reviewed: 05.07.2025
In medicine, the term "fibroelastosis" refers to changes in the connective tissue of the body covering the surface of internal organs and blood vessels caused by a disruption in the growth of elastic fibers. At the same time, thickening of the walls of organs and their structures is noted, which necessarily affects the functioning of vital systems of the body, in particular the cardiovascular and respiratory systems. This in turn entails a deterioration in the patient's well-being, especially during physical exertion, affecting the quality and duration of life.
Epidemiology
In general, diseases accompanied by changes in connective tissue, resulting in thickening of the membranes and partitions of internal organs, can be divided into 2 groups: cardiac fibroelastosis and pulmonary fibroelastosis. Heart pathology can be both congenital and acquired; in the pulmonary form of the disease, we are talking about an acquired disease.
Pulmonary fibroelastosis begins to develop in middle age (closer to 55-57 years), although in half of the cases the origin of the disease must be sought in childhood. A "light" period is characteristic, when symptoms of the disease are absent. At the same time, the disease has no gender preferences and can equally affect both women and men. This rather rare pathology is characterized by changes in the tissues of the pleura and parenchyma (functional cells) of the lung, mainly in the upper lobe of the lung. Since the etiology and pathogenesis of the disease remain unclear, the disease is classified as an idiopathic pathology. According to medical terminology, it is called "pleuroparenchymatous fibroelastosis". [ 1 ]
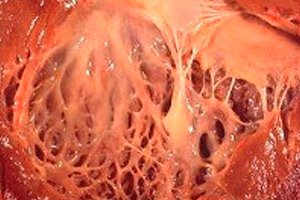
Cardiac fibroelastosis is a generalized name for a pathology of the cardiac membranes, characterized by their thickening and decreased functionality. Congenital forms of the pathology are characterized by diffuse (widespread) thickening of the inner membrane of the heart. This is a thin connective tissue lining the cavity of the heart (its sections) and forming its valves.
In adult patients, a focal form of the disease is usually diagnosed, when the inner surface of the heart seems to be covered with patches of stronger and thicker tissue (it may include not only overgrown fibers, but also thrombotic masses).
In half of the cases of cardiac fibroelastosis, not only the organ wall becomes thicker, but also the valves (bicuspid mitral between the atrium and ventricle of the same name, tricuspid aortic between the left ventricle and aorta, pulmonary between the right ventricle and pulmonary artery). This in turn can disrupt the functioning of the valves and cause narrowing of the arterial orifice, which is already small compared to other cavities of the heart.
In medical terminology, endocardial fibroelastosis is called endocardial fibroelastosis (prenatal fibroelastosis, endocardial sclerosis, fetal endocarditis, etc.). But quite often the middle muscular layer of the cardiac membrane can also be involved in the process. [ 2 ]
Anomalies in the structure of the myocardium (the muscular layer of the heart, consisting of cardiomyocytes), gene mutations and severe infectious processes can cause a common form of fibroelastosis, when not only the endocardium but also the myocardium are involved in the process. Usually, dysplastic processes in the endocardium, caused by various reasons, occur at the border of its contact with the muscular membrane, disrupting the contractility of this layer. In some cases, there is even ingrowth of the inner layer into the myocardium, replacement of cardiomyocytes with fibroblasts and fibers, which affects the conductivity of nerve impulses and the rhythmic work of the heart.
Compression of the blood vessels in the thickness of the cardiac membrane by the thickened myocardium disrupts the nutrition of the myocardium (myocardial ischemia), which in turn can lead to necrosis of the tissues of the heart muscle.
Endocardial fibroelastosis with damage to the myocardium of the heart is called subendocardial or endomyocardial fibroelastosis.
According to statistics, in most cases of this rare disease (only 0.007% of the total number of newborns), fibroelastosis of the left ventricle of the heart is diagnosed, although in some cases the process also spreads to the right ventricle and atria, including the valves separating them.
Cardiac fibroelastosis is often accompanied by damage to large coronary vessels, also covered with connective tissue. In adulthood, it often occurs against the background of progressive vascular atherosclerosis.
The disease is more often registered in tropical African countries among populations with a low standard of living, which is facilitated by poor nutrition, frequent infections, and certain foods and plants consumed as food.
Endocardial thickening is also observed in the last stage of Löffler's fibroplastic endocarditis, which mainly affects middle-aged men. The pathogenesis of this disease is also associated with infectious agents that cause the development of severe eosinophilia, which is more typical for internal parasitic infections. In this case, the body's tissues (primarily the heart muscle and brain) begin to experience a lack of oxygen (hypoxia). Despite the similarity of the symptoms of cardiac fibroelastosis and Löffler's fibrous endocarditis, doctors consider them to be completely different diseases.
Causes fibroelastosis
Fibroelastosis refers to changes in connective tissue in vital organs: the heart and lungs, which is accompanied by disruption of organ function and is reflected in the patient's appearance and condition. Doctors have known about the disease for decades. Fibroelastosis of the inner lining of the heart (endocardium) was described back in the early 18th century, and similar changes in the lungs began to be discussed 2 and a half centuries later. However, doctors have not yet reached a final agreement on the causes of the pathological proliferation of connective tissue.
It remains unclear what exactly causes the disruption of growth and development of connective fibers. But scientists identify certain risk factors for such changes, considering them possible (but not final) causes of the disease.
Thus, in the pathogenesis of pulmonary fibroelastosis, which is considered a disease of mature people, a special role is given to recurrent infectious lesions of the organ, which are found in half of the patients. Infections provoke inflammation of the lung tissue and pleura, and long-term inflammation predisposes to their fibrous transformation.
Some patients have a family history of fibroelastosis, suggesting a hereditary predisposition. Non-specific autoantibodies have been found in their bodies, which provoke long-term inflammatory processes of uncertain etiology.
There is an opinion that fibrous changes in lung tissue can be caused by gastroesophageal reflux disease. Although this connection is most likely indirect. It is also believed that the risk of fibroelastosis is higher in those who suffer from cardiovascular diseases or pulmonary thrombosis.
Pulmonary fibroelastosis in young and adolescent age may remind of itself during pregnancy. Usually the disease is hidden for about 10 years or more, but it may manifest itself earlier, possibly due to the increased load on the body of the expectant mother and hormonal changes, but there is no exact explanation yet. Nevertheless, a similar picture of the development of the disease was observed in 30% of the examined patients of reproductive age.
Pregnancy itself cannot cause the disease, but it can accelerate the development of events, which is very sad, because the mortality rate of the disease is very high, and life expectancy with fibroelastosis is short.
In most cases, cardiac fibroelastosis can be attributed to childhood diseases. Congenital pathology is detected in the prenatal period in a 4-7-month-old fetus, but the diagnosis can only be confirmed after the child is born. Several possible negative factors are considered in the pathogenesis of this form of the disease: infectious and inflammatory diseases of the mother transmitted to the fetus, abnormalities in the development of the heart membranes, impaired blood supply to the heart tissue, genetic mutations, oxygen deficiency.
It is believed that among infections, viruses make the greatest pathogenetic contribution to the development of cardiac fibroelastosis, because they are embedded in the body's cells, destroy them, and change the properties of tissues. The unformed immune system of the fetus cannot provide it with protection from these pathogens, unlike the immunity of the expectant mother. The latter may not experience the consequences of a viral infection, while in the fetus, an intrauterine infection can provoke the appearance of various anomalies.
Some scientists believe that the decisive role in the pathogenesis of the infectious form of fibroelastosis is played by an infection affecting the fetus up to 7 months of age. Later, it can only cause inflammatory diseases of the heart (myocarditis, endocarditis).
Anomalies in the development of the membranes and valves of the heart can be provoked by both the inflammatory process and inadequate autoimmune reactions, as a result of which the cells of the immune system begin to attack the body's own cells.
Gene mutations cause abnormal development of connective tissue, because genes contain information about the structure and behavior of protein structures (in particular, collagen and elastin proteins).
Hypoxia and ischemia of cardiac tissue may be a consequence of abnormal heart development. In this case, we speak of secondary fibroelastosis, provoked by congenital heart defects (CHD). These include such anomalies that cause obstruction (impaired patency of the heart and its vessels):
- stenosis or narrowing of the aorta near the valve,
- coarctation or segmental narrowing of the aorta at the junction of its arch and descending section,
- atresia or absence of a natural opening in the aorta,
- underdevelopment of heart tissue (most often the left ventricle, less often the right ventricle and atria), which affects the pumping function of the heart.
There is an opinion that toxicosis during pregnancy can also act as a predisposing factor for fibroelastosis in the fetus.
In the postnatal period, the development of cardiac fibroelastosis can be facilitated by infectious and inflammatory diseases of the organ membranes, hemodynamic disorders as a result of injuries, vascular thromboembolism, myocardial hemorrhage, metabolic disorders (increased fibrin formation, protein and iron metabolism disorders: amyloidosis, hemochromatosis). The same reasons cause the development of the disease in adults.
Pathogenesis
Connective tissue is a special tissue of the human body that is part of almost all organs, but does not actively participate in their functions. Connective tissue is credited with supporting and protective functions. Forming a kind of skeleton (framework, stroma) and limiting the functional cells of the organ, it ensures its final shape and size. Having sufficient strength, connective tissue also protects the organ cells from destruction and injury, prevents the penetration of pathogens, and with the help of special macrophage cells absorbs obsolete structures: dead tissue cells, foreign proteins, waste blood components, etc.
This tissue can be called auxiliary, because it does not contain cellular elements that ensure the functionality of one or another organ. Nevertheless, its role in the life of the body is quite large. Being part of the membranes of blood vessels, connective tissue ensures the safety and functionality of these structures, due to which nutrition and respiration (trophism) of the surrounding tissues of the internal environment of the body are carried out.
There are several types of connective tissue. The membrane covering the internal organs is called loose connective tissue. It is a semi-liquid, colorless substance containing wavy collagen fibers and straight elastin fibers, between which various types of cells are randomly scattered. Some of these cells (fibroblasts) are responsible for the formation of fibrous structures, others (endotheliocytes and mast cells) form a translucent matrix of connective tissue and produce special substances (heparin, histamine), others (macrophages) provide phagocytosis, etc.
The second type of fibrous tissue is dense connective tissue, which does not contain a large number of individual cells, which in turn is divided into white and yellow. White tissue consists of tightly packed collagen fibers (ligaments, tendons, periosteum), and yellow tissue consists of chaotically intertwined elastin fibers with inclusions of fibroblasts (part of ligaments, membranes of blood vessels, lungs).
Connective tissues also include: blood, fat, bone and cartilage tissue, but we are not interested in them yet, since, speaking of fibroelastosis, we mean changes in fibrous structures. And elastic and resilient fibers are contained only in loose and dense connective tissues.
The synthesis of fibroblasts and the formation of connective tissue fibers from them is regulated at the brain level. This ensures the constancy of its characteristics (strength, elasticity, thickness). If, due to some pathological reasons, the synthesis and development of auxiliary tissue is disrupted (the number of fibroblasts increases, their "behavior" changes), there is an proliferation of strong collagen fibers or a change in the growth of elastic ones (they remain short, twist), which leads to a change in the properties of the organ membrane and some internal structures covered with connective tissue. They acquire a greater than necessary thickness, become denser, stronger and inelastic, resembling fibrous tissue in ligaments and tendons, which requires great effort to stretch.
Such tissue does not stretch well, limiting the organ's movements (automatic rhythmic movements of the heart and blood vessels, changes in the size of the lungs during inhalation and exhalation), hence the disruption of the blood supply and respiratory organs, leading to oxygen deficiency.
The fact is that the blood supply of the body is carried out thanks to the heart, which works as a pump, and two circles of blood circulation. The pulmonary circulation is responsible for blood supply and gas exchange in the lungs, from where oxygen is delivered to the heart with the blood flow, and from there to the systemic circulation and distributed throughout the body, providing respiration to organs and tissues.
The elastic membrane, limiting the contraction of the heart muscle, reduces the functionality of the heart, which does not pump blood as actively, and with it oxygen. With fibroelastosis of the lungs, their ventilation (osigenation) is impaired, it is clear that less oxygen begins to enter the blood, which, even with normal heart function, will contribute to oxygen starvation (hypoxia) of tissues and organs. [ 3 ]
Symptoms fibroelastosis
Cardiac and pulmonary fibroelastosis are two types of disease characterized by a disorder of fiber synthesis in connective tissue. They have different localizations, but both are potentially life-threatening, as they are associated with progressive or severe cardiac and respiratory failure.
Pulmonary fibroelastosis is a rare type of interstitial disease of this important organ of the respiratory system. These include chronic pathologies of the lung parenchyma with damage to the alveolar walls (inflammation, disruption of their structure and structure), the inner lining of the pulmonary capillaries, etc. Fibroelastosis is often considered a special rare form of progressive pneumonia with a tendency to fibrous changes in the tissues of the lung and pleura.
It is almost impossible to detect the disease at the very beginning, because it may not remind of itself for about 10 years. This period is called the clear interval. The onset of pathological changes that do not yet affect the volume of the lungs and gas exchange can be detected by chance, during a detailed examination of the lungs in connection with another disease of the respiratory system or injury.
The disease is characterized by a slow progression of symptoms, so the first manifestations of the disease can be significantly delayed in time from its onset. The symptoms intensify gradually.
The first signs of the disease that are worth paying attention to are coughing and increasing shortness of breath. Such symptoms often become a consequence of a previous respiratory disease, so they can be associated with a cold and its consequences for a long time. Shortness of breath is often perceived as a cardiac disorder or age-related changes. After all, the disease is diagnosed in people approaching old age.
Mistakes can be made by both patients and doctors examining them, which leads to late detection of a dangerous disease. It is worth paying attention to the cough, which is unproductive in fibroelastosis, but is not stimulated by mucolytics and expectorants, but is stopped by antitussives. A prolonged cough of this nature is a characteristic symptom of pulmonary fibroelastosis.
Dyspnea is caused by progressive respiratory failure due to thickening of the alveolar walls and pleura, a decrease in the volume and number of alveolar cavities in the lung (the parenchyma of the organ is visible on an X-ray as a honeycomb). The symptom intensifies under the influence of physical exertion, first significant, and then even small. As the disease progresses, it worsens, which causes disability and death of the patient.
The progression of fibroelastosis is accompanied by a deterioration in the general condition: hypoxia leads to weakness and dizziness, body weight decreases (anorexia develops), the nail phalanges change to the type of drumsticks, the skin becomes pale and has a sickly appearance.
Half of the patients develop non-specific symptoms such as difficulty breathing and chest pain, characteristic of pneumothorax (accumulation of gases in the pleural cavity). This anomaly can also occur as a result of injuries, primary and secondary lung diseases, improper treatment, so it cannot be diagnosed.
Cardiac fibroelastosis, as well as the pathology of connective tissue growth in the lungs, is characterized by: pale skin, weight loss, weakness, which is often paroxysmal, shortness of breath. Persistent subfebrile temperature without signs of a cold or infection may also be observed.
Many patients experience changes in liver size. It increases in size without symptoms of dysfunction. Swelling of the legs, face, arms, and sacral region is also possible.
A characteristic manifestation of the disease is considered to be increasing circulatory failure associated with disruption of the heart. In this case, tachycardia is diagnosed (increased heart rate, often combined with arrhythmia), shortness of breath (including in the absence of physical activity), tissue cyanosis (bluish coloration caused by the accumulation of carboxyhemoglobin in the blood, i.e. a compound of hemoglobin with carbon dioxide due to disrupted blood flow, and accordingly gas exchange).
In this case, symptoms may appear either immediately after the birth of a child with this pathology, or over a period of time. When older children and adults are affected, signs of severe heart failure usually appear against the background of a respiratory infection, which acts as a trigger. [ 4 ]
Fibroelastosis in children
If pulmonary fibroelastosis is a disease of adults, often originating in childhood, but not making itself known for a long time, then a similar pathology of the endocardium of the heart often appears even before the birth of the baby and affects his life from the first moments of birth. This rare but severe pathology is the cause of the development of difficult-to-correct heart failure in infants, many of whom die within 2 years. [ 5 ]
Endocardial fibroelastosis in newborns is in most cases the result of pathological processes occurring in the baby's body during prenatal age. Infections received from the mother, genetic mutations, abnormalities in the development of the cardiovascular system, hereditary metabolic diseases - all this, according to scientists, can lead to changes in the connective tissue in the membranes of the heart. Especially if a 4-7-month-old fetus is exposed to two or more factors at the same time.
For example, a combination of abnormalities in the development of the heart and coronary vessels (stenosis, atresia, coarctation of the aorta, abnormal development of myocardial cells, endocardial weakness, etc.), which contribute to tissue ischemia, combined with an inflammatory process due to infection, leaves the child with virtually no chance of more or less survival. While organ development defects can still be promptly corrected, progressive fibroelastosis can only be slowed down, but not cured.
Usually, cardiac fibroelastosis in the fetus is detected already during pregnancy during ultrasound diagnostics in the second or third trimester. Ultrasound and echocardiography at 20 to 38 weeks showed hyperechogenicity, which indicates thickening and compaction of the endocardium (usually diffuse, less often focal), a change in the size and shape of the heart (the organ is enlarged and takes the shape of a ball or bullet, the internal structures are gradually smoothed out). [ 6 ]
In 30-35% of cases, fibroelastosis was detected before 26 weeks of pregnancy, in 65-70% - in the subsequent period. In more than 80% of newborns, fibroelastosis is combined with obstructive heart defects, i.e. it is secondary, despite the early stages of its detection. Left ventricular hyperplasia was detected in half of the affected children, which explains the high prevalence of fibroelastosis of this particular heart structure. Pathologies of the aorta and its valve, determined in a third of children with endocardial proliferation, also lead to an increase (dilation) of the left ventricular chamber and a disruption of its functionality.
In case of instrumentally confirmed cardiac fibroelastosis, doctors recommend terminating the pregnancy. In almost all children born whose mothers refused a medical abortion, the signs of the disease were confirmed. Symptoms of heart failure, characteristic of fibroelastosis, appear within a year (rarely in the 2nd-3rd year of life). In children with a combined form of the disease, signs of heart failure are detected from the first days of life.
Congenital forms of primary and combined fibroelastosis in children most often have a rapid course with the development of severe heart failure. Low activity, lethargy of the child, refusal to breastfeed due to rapid fatigue, poor appetite, increased sweating indicate ill health. All this leads to the fact that the child does not gain weight well. The baby's skin is painfully pale, in some with a bluish tint, most often in the nasolabial triangle.
There are signs of poor immunity, so such children often and quickly catch respiratory infections, complicating the situation. Sometimes in the first days and months of life, the child does not show any circulatory disorders, but frequent infections and lung diseases become a trigger for the development of congestive heart failure.
Additional health examinations of newborns and young children with suspected fibroelastosis or previously diagnosed showed low blood pressure (hypotension), enlarged heart size (cardiomegaly), muffled tones when listening to the heart, sometimes systolic murmur characteristic of mitral valve insufficiency, tachycardia, dyspnea. Listening to the lungs shows the presence of wheezing, indicating congestion.
Endocardial damage to the left ventricle often leads to weakening of the muscular layer of the heart (myocardium). The normal heart rhythm consists of two rhythmically alternating tones. With fibroelastosis, a third (and sometimes a fourth) tone may appear. Such a pathological rhythm is clearly audible and resembles a three-beat gait of a horse (gallop) in its sound, which is why it is called the gallop rhythm.
Another symptom of fibroelastosis in young children is the appearance of a cardiac hump. The fact is that the child's ribs in the early postnatal period remain non-ossified and are represented by cartilaginous tissue. The increase in the size of the heart leads to the fact that it begins to press on the "soft" ribs, as a result of which they bend and take a permanent forward-curved shape (cardiac hump). With fibroelastosis in adults, a cardiac hump does not form due to the strength and rigidity of the bone tissue of the ribs, even in the case of an increase in all structures of the heart.
The formation of a cardiac hump in itself indicates only a congenital heart defect without specifying its nature. But in any case, it is associated with an increase in the size of the heart and its ventricles.
Edema syndrome in fibroelastosis in children is rarely diagnosed, but many children experience an enlarged liver, which begins to protrude by an average of 3 cm from under the edge of the costal arch.
If fibroelastosis is acquired (for example, it is a consequence of inflammatory diseases of the heart membranes), the clinical picture is most often slowly progressive. For some time, symptoms may be absent altogether, then weak signs of heart dysfunction appear in the form of shortness of breath during physical exertion, increased heart rate, rapid fatigue and low physical endurance. A little later, the liver begins to enlarge, edema and dizziness appear.
All symptoms of acquired fibroelastosis are non-specific, which complicates the diagnosis of the disease, resembling cardiomyopathy, liver and kidney disease. The disease is most often diagnosed at the stage of severe heart failure, which negatively affects the results of treatment.
Complications and consequences
It should be said that fibroelastosis of the heart and lungs are serious pathologies, the course of which depends on various circumstances. Congenital heart defects significantly complicate the situation, which can be surgically eliminated at an early age, but at the same time there remains a fairly high risk of death (approximately 10%).
It is believed that the earlier the disease develops, the more severe its consequences will be. This is confirmed by the fact that congenital fibroelastosis in most cases has a fulminant or acute course with rapid progression of heart failure. The development of acute heart failure in a child under 6 months is considered a bad prognostic sign.
However, the treatment does not guarantee full restoration of cardiac function, but only slows down the progression of symptoms of heart failure. On the other hand, the absence of such supportive treatment leads to death within the first two years of the baby's life.
If heart failure is detected in the first days and months of a baby's life, the child will most likely not survive even a week. The response to treatment varies among children. In the absence of a therapeutic effect, there is virtually no hope. But with the help provided, the life expectancy of a sick child is short (from several months to several years).
Surgery and correction of congenital heart defects that caused fibroelastosis usually improve the patient's condition. With successful surgical treatment of left ventricular hyperplasia and compliance with the doctor's requirements, the disease may acquire a benign course: heart failure will have a chronic course without signs of progression. Although the hope for such a result is small.
As for the acquired form of cardiac fibroelastosis, it quickly becomes chronic and gradually progresses. Medication can slow down the process, but not stop it.
Pulmonary fibroelastosis, regardless of the time of appearance of changes in the parenchyma and membranes of the organ after the light period, begins to progress rapidly and actually kills a person in a couple of years, causing severe respiratory failure. The sad thing is that effective methods of treating the disease have not yet been developed. [ 7 ]
Diagnostics fibroelastosis
Endomyocardial fibroelastosis, the symptoms of which are detected in most cases at an early age, is a congenital disease. If we exclude those rare cases when the disease began to develop in late childhood and adulthood as a complication of injuries and somatic diseases, it is possible to identify the pathology in the prenatal period, i.e. before the birth of the child.
Doctors believe that pathological changes in the endocardial tissues, changes in the shape of the fetal heart and some features of its functioning, characteristic of fibroelastosis, can be determined as early as the 14th week of pregnancy. But this is still a fairly short period, and it cannot be ruled out that the disease may manifest itself somewhat later, closer to the third trimester of pregnancy, and sometimes a couple of months before delivery. That is why, when monitoring pregnant women, it is recommended to conduct clinical ultrasound screenings of the fetal heart at intervals of several weeks.
By what signs can doctors suspect the disease during the next ultrasound? Much depends on the form of the disease. Most often, fibroelastosis is diagnosed in the area of the left ventricle, but this structure is not always enlarged. The dilated form of the disease with an enlarged left ventricle of the heart is easily determined during an ultrasound examination by the spherical shape of the heart, the apex of which is represented by the left ventricle, the general increase in the size of the organ, and the bulging of the interventricular septum towards the right ventricle. But the main sign of fibroelastosis is thickening of the endocardium, as well as cardiac septa with a characteristic increase in the echogenicity of these structures, which is determined by a specific ultrasound examination.
The study is conducted using special ultrasound equipment with cardiology programs. Fetal echocardiography does not harm the mother or the unborn child, but allows not only to identify anatomical changes in the heart, but also to determine the condition of the coronary vessels, the presence of blood clots in them, and changes in the thickness of the cardiac membranes.
Fetal echocardiography is prescribed not only in the presence of deviations during the decoding of ultrasound results, but also in the case of a mother’s infection (especially viral), taking potent medications, hereditary predisposition, the presence of metabolic disorders, as well as congenital cardiac pathologies in older children.
Fetal echocardiography can also detect other congenital forms of fibroelastosis. For example, fibroelastosis of the right ventricle, a widespread process with simultaneous damage to the left ventricle and adjacent structures: the right ventricle, heart valves, atria, combined forms of fibroelastosis, endomyocardial fibroelastosis with thickening of the inner lining of the ventricles and involvement of part of the myocardium in the pathological process (usually combined with thrombosis of the wall).
Endocardial fibroelastosis detected at prenatal age has a very poor prognosis, so doctors recommend terminating the pregnancy in this case. The possibility of an erroneous diagnosis is excluded by a repeated ultrasound of the fetal heart, which is carried out 4 weeks after the first examination that revealed the pathology. It is clear that the final decision on terminating or maintaining the pregnancy remains with the parents, but they must be aware of what kind of life they are condemning the child to.
Endocardial fibroelastosis is not always detected during pregnancy, especially considering the fact that not all expectant mothers register with a women's health clinic and undergo preventive ultrasound diagnostics. The illness of the child in her womb has virtually no effect on the condition of the pregnant woman, so the birth of a sick baby often becomes an unpleasant surprise.
In some cases, both parents and doctors learn about the baby's illness several months after the child's birth. In this case, laboratory blood tests may show nothing, except for an increase in sodium concentration (hypernatremia). But their results will be useful in conducting differential diagnostics to exclude inflammatory diseases.
There is still hope for instrumental diagnostics. A standard study of the heart (ECG) is not particularly indicative in the case of fibroelastosis. It helps to identify disturbances in the heart and electrical conductivity of the heart muscle, but does not specify the causes of such disorders. Thus, a change in the ECG voltage (at a younger age it is usually understated, at an older age - on the contrary, excessively high) indicates cardiomyopathy, which can be associated not only with heart pathologies, but also with metabolic disorders. Tachycardia is a symptom of cardiac diseases. And if both ventricles of the heart are affected, the cardiogram may generally seem normal. [ 8 ]
Computed tomography (CT) is an excellent noninvasive tool for detecting cardiovascular calcification and excluding pericarditis.[ 9 ]
Magnetic resonance imaging (MRI) may be useful in detecting fibroelastosis because biopsy is invasive. A hypointense rim on a myocardial perfusion sequence and a hyperintense rim on a delayed enhancement sequence are suggestive of fibroelastosis.[ 10 ]
But this does not mean that the study should be abandoned, because it helps to determine the nature of the heart's work and the degree of developing heart failure.
When symptoms of heart failure appear and the patient consults a doctor about this, the patient is also prescribed: chest X-ray, computed tomography or magnetic resonance imaging of the heart, echocardiography (EchoCG). In doubtful cases, it is necessary to resort to a biopsy of heart tissue with subsequent histological examination. The diagnosis is very serious, therefore it requires the same approach to diagnosis, although the treatment is not much different from symptomatic therapy for coronary heart disease and heart failure.
But even such a scrupulous examination will not be useful if its results are not used in differential diagnostics. ECG results can be used to differentiate acute fibroelastosis from idiopathic myocarditis, exudative pericarditis, aortic stenosis. At the same time, laboratory tests will not show signs of inflammation (leukocytosis, increased ESR, etc.), and temperature measurements will not show hyperthermia.
Analysis of heart sounds and murmurs, changes in the size of the atria, and a study of the anamnesis help to distinguish endocardial fibroelastosis from isolated mitral valve insufficiency and mitral valve defect.
Analysis of anamnestic data is useful in distinguishing between fibroelastosis and the heart and aortic stenosis. In case of aortic stenosis, it is also worth paying attention to the preservation of sinus rhythm and the absence of thromboembolism. Heart rhythm disturbances and thrombus deposition are not observed in exudative pericarditis either, but the disease manifests itself with an increase in temperature and fever.
The greatest difficulty is in differentiating endocardial fibroelastosis and congestive cardiomyopathy. In this case, fibroelastosis, although in most cases not accompanied by pronounced cardiac conduction disorders, has a less favorable treatment prognosis.
In case of combined pathologies, it is necessary to pay attention to any deviations revealed during a tomogram or ultrasound of the heart, because congenital defects significantly complicate the course of fibroelastosis. If combined endocardial fibroelastosis is detected in the intrauterine period, it is inappropriate to maintain the pregnancy. It is much more humane to terminate it.
Diagnosis of pulmonary fibroelastosis
Diagnosis of pulmonary fibroelastosis also requires certain knowledge and skills from the doctor. The fact is that the symptoms of the disease are quite heterogeneous. On the one hand, they indicate congestive lung diseases (non-productive cough, shortness of breath), and on the other hand, they may also be a manifestation of cardiac pathology. Therefore, diagnosis of the disease cannot be reduced to only stating symptoms and auscultation.
Blood tests of the patient help to exclude inflammatory lung diseases, but do not provide information on quantitative and qualitative changes in tissues. The presence of signs of eosinophilia helps to differentiate the disease from pulmonary fibrosis, which is similar in manifestations, but does not reject or confirm the fact of fibroelastosis.
Instrumental studies are considered more indicative: chest X-ray and tomographic examination of the respiratory organs, as well as functional analyses, which consist of determining respiratory volumes, vital capacity of the lungs, and pressure in the organ.
In case of pulmonary fibroelastosis, it is worth paying attention to the decrease in the function of external respiration, measured during spirometry. The decrease in active alveolar cavities significantly affects the vital capacity of the lungs (VCL), and the thickening of the walls of internal structures affects the diffusion capacity of the organ (DCL), which ensures ventilation and gas exchange functions (in simple terms, absorbing carbon dioxide from the blood and giving off oxygen).
Characteristic signs of pleuroparenchymal fibroelastosis are a combination of limited air flow into the lungs (obstruction) and impaired lung expansion during inhalation (restriction), deterioration of external respiratory function, moderate pulmonary hypertension (increased pressure in the lungs), diagnosed in half of patients.
A lung tissue biopsy shows characteristic changes in the internal structure of the organ. These include: fibrosis of the pleura and parenchyma in combination with elastosis of the alveolar walls, accumulation of lymphocytes in the area of compacted alveolar septa, transformation of fibroblasts into muscle tissue that is not typical for them, and the presence of edematous fluid.
The tomogram shows damage to the lungs in the upper sections in the form of foci of pleural compaction and structural changes in the parenchyma. The enlarged connective tissue of the lungs resembles muscle tissue in color and properties, but the volume of the lungs decreases. Quite large air-containing cavities (cysts) are found in the parenchyma. Irreversible focal (or diffuse) expansion of the bronchi and bronchioles (traction bronchiectasis) and a low position of the diaphragm dome are characteristic.
Radiological examinations reveal areas of "ground glass" and "honeycomb lung" in many patients, indicating uneven ventilation of the lungs due to the presence of foci of tissue compaction. Approximately half of patients have enlarged lymph nodes and liver.
Pulmonary fibroelastosis should be differentiated from fibrosis caused by parasitic infection and associated eosinophilia, endocardial fibroelastosis, lung diseases with impaired ventilation and a "honeycomb lung" picture, the autoimmune disease histicotitis X (one form of this pathology with lung damage is called Hand-Schüller-Christian disease), manifestations of sarcoidosis and pulmonary tuberculosis.
Treatment fibroelastosis
Fibroelastosis, no matter where it is located, is considered a dangerous and practically incurable disease. Pathological changes in the pleura and lung parenchyma cannot be restored with medication. And even the use of hormonal anti-inflammatory drugs (corticosteroids) in combination with bronchodilators does not give the desired result. Bronchodilators help to alleviate the patient's condition a little, relieving the obstructive syndrome, but they do not affect the processes occurring in the lungs, so they can only be used as a supportive therapy.
Surgical treatment for pulmonary fibroelastosis is also ineffective. The only operation that could change the situation is a donor organ transplant. But lung transplantation, alas, has the same unfavorable prognosis. [ 11 ]
According to foreign scientists, fibroelastosis can also be considered as one of the frequent complications of lung or bone marrow stem cell transplantation. In both cases, changes occur in the connective tissue fibers of the lungs, affecting the function of external respiration.
The disease progresses without treatment (and effective treatment is currently absent), and about 40% of patients die from respiratory failure within 1.5-2 years. The life expectancy of those who remain is also severely limited (up to 10-20 years), as is their ability to work. The person becomes disabled.
Cardiac fibroelastosis is also considered a medically incurable disease, especially if it is a congenital pathology. Usually, children do not live to be 2 years old. They can only be saved by a heart transplant, which in itself is a difficult operation with a high degree of risk and unpredictable consequences, especially at such a young age.
In some babies, it is possible to correct congenital heart defects surgically so that they do not worsen the condition of the sick child. In case of stenosis of the artery, a vascular dilator is installed - a shunt (aortocoronary bypass). In case of dilation of the left ventricle of the heart, its shape is quickly restored. But even such an operation does not guarantee that the child will be able to do without a transplant. About 20-25% of babies survive, and they suffer from heart failure all their lives, i.e. they are not considered healthy.
If the disease is acquired, it is worth fighting for the child's life with the help of medications. But it is important to understand that the earlier the disease manifests itself, the harder it will be to fight it.
Drug treatment is aimed at combating and preventing exacerbations of heart failure. Patients are prescribed the following cardiac drugs:
- angiotensin-converting enzyme (ACE) inhibitors, which affect blood pressure and maintain it within normal limits (captopril, enalapril, benazepril, etc.),
- beta-blockers used to treat heart rhythm disorders, arterial hypertension, and prevent myocardial infarction (anaprilin, bisoprolol, metoprolol),
- cardiac glycosides, which, when used over a long period of time, not only support the functioning of the heart (increase the potassium content in cardiomyocytes and improve myocardial conductivity), but are also able to somewhat reduce the degree of endocardial thickening (digoxin, gitoxin, strophanthin),
- potassium-sparing diuretics (spironolactone, veroshpiron, decriz), preventing tissue edema,
- antithrombotic therapy with anticoagulants (cardiomagnyl, magnicor), preventing the formation of blood clots and circulatory disorders in the coronary vessels.
In the congenital form of endocardial fibroelastosis, supportive treatment does not promote recovery, but reduces the risk of death from heart failure or thromboembolism by 70-75%. [ 12 ]
Medicines
As we can see, the treatment of endocardial fibroelastosis is practically no different from that of heart failure. In both cases, cardiologists take into account the severity of cardiopathy. Prescribing medications is strictly individual, taking into account the patient's age, concomitant diseases, form and degree of heart failure.
In the treatment of acquired endocardial fibroelastosis, drugs of 5 groups are used. Let's consider one drug from each group.
"Enalapril" is a drug from the group of ACE inhibitors, produced in the form of tablets of various dosages. The drug increases coronary blood flow, dilates arteries, reduces blood pressure without affecting cerebral circulation, slows down and reduces the expansion of the left ventricle of the heart. The drug improves blood supply to the myocardium, reducing the effects of ischemia, slightly reduces blood clotting, preventing the formation of blood clots, has a slight diuretic effect.
In case of heart failure, the medicine is prescribed for a period of more than six months or on a permanent basis. The medicine is started with a minimum dose (2.5 mg), gradually increasing it by 2.5-5 mg every 3-4 days. The permanent dose will be the one that is well tolerated by the patient and maintains blood pressure within the normal range.
The maximum daily dose is 40 mg. It can be taken once or divided into 2 doses.
If blood pressure is below normal, the dose is gradually reduced. Treatment with Enalapril should not be stopped abruptly. It is recommended to take a maintenance dose of 5 mg per day.
The drug is intended for the treatment of adult patients, but can also be prescribed to a child (safety has not been officially established, but in the case of fibroelastosis, the life of a small patient is at stake, so the risk ratio is taken into account). The ACE inhibitor is not prescribed to patients with intolerance to the components of the drug, with porphyria, pregnancy and during breastfeeding. If the patient has previously had Quincke's edema while taking any drugs of this group, Enalapril is prohibited.
Caution should be exercised when prescribing the drug to patients with concomitant pathologies: severe kidney and liver diseases, hyperkalemia, hyperaldosteronism, aortic or mitral valve stenosis, systemic connective tissue pathologies, cardiac ischemia, brain disease, diabetes mellitus.
When treating with the drug, do not take conventional diuretics to avoid dehydration and a strong hypotensive effect. Simultaneous administration with potassium-sparing diuretics requires dose adjustment, since there is a high risk of hyperkalemia, which in turn provokes cardiac arrhythmia, seizures, decreased muscle tone, increased weakness, etc.
The drug "Enalapril" is usually well tolerated, but some patients may experience side effects. The most common are: a strong decrease in blood pressure up to collapse, headaches and dizziness, sleep disorders, increased fatigue, reversible loss of balance, hearing and vision, the appearance of tinnitus, shortness of breath, coughing without sputum secretion, changes in the composition of the blood and urine, usually indicating improper functioning of the liver and kidneys. Possible: hair loss, decreased sexual desire, symptoms of "hot flashes" (feeling of heat and palpitations, hyperemia of the skin of the face, etc.).
"Bisoprolol" is a beta-blocker with selective action, which has hypotensive and anti-ischemic effects, helps to combat the manifestations of tachycardia and arrhythmia. A budget drug in the form of tablets, preventing the progression of heart failure in endocardial fibroelastosis. [ 13 ]
Like many other drugs prescribed for coronary heart disease and CHF, Bisoprolol is prescribed for a long time. It is advisable to take it in the morning before or during meals.
As for the recommended dosages, they are selected individually depending on the blood pressure readings and the drugs that are prescribed in parallel with this medicine. On average, a single (also daily) dose is 5-10 mg, but with a slight increase in pressure it can be reduced to 2.5 mg. The maximum dose that can be prescribed to a patient with normally functioning kidneys is 20 mg, but only with consistently high blood pressure.
Increasing the indicated dosages is possible only with the permission of a doctor. But in case of severe liver and kidney diseases, 10 mg is considered the maximum permissible dose.
In the complex treatment of heart failure against the background of left ventricular dysfunction, which most often occurs with fibroelastosis, an effective dose is selected by gradually increasing the dosage by 1.25 mg. In this case, they start with the minimum possible dose (1.25 mg). The dosage is increased at intervals of 1 week.
When the dose reaches 5 mg, the interval is increased to 28 days. After 4 weeks, the dose is increased by 2.5 mg. Adhering to this interval and norm, they reach 10 mg, which the patient will have to take for a long time or constantly.
If such a dosage is poorly tolerated, it is gradually reduced to a comfortable level. Stopping treatment with a beta-blocker should also not be abrupt.
The drug should not be prescribed in case of hypersensitivity to the active and auxiliary substances of the drug, acute and decompensated heart failure, cardiogenic shock, atrioventricular block grades 2-3, bradycardia, consistently low blood pressure and some other heart pathologies, severe bronchial asthma, broncho-obstruction, severe peripheral circulatory disorders, metabolic acidosis.
Caution should be exercised when prescribing complex treatment. Thus, the combination of Bisoprolol with some antiarrhythmic drugs (quinidine, lidocaine, phenytoin, etc.), calcium antagonists and central hypotensive drugs is not recommended.
Unpleasant symptoms and disorders that are possible during treatment with Bisoprolol: increased fatigue, headaches, hot flashes, sleep disorders, drop in blood pressure and dizziness when getting out of bed, hearing loss, gastrointestinal symptoms, liver and kidney disorders, decreased potency, muscle weakness and cramps. Sometimes patients complain of peripheral circulatory disorders, which manifests itself in the form of a decrease in temperature or numbness of the extremities, especially the fingers and toes.
In the presence of concomitant diseases of the bronchopulmonary system, kidneys, liver, and diabetes mellitus, the risk of adverse effects is higher, which indicates an exacerbation of the disease.
"Digoxin" is a popular budget cardiac glycoside based on the foxglove plant, which is dispensed strictly by prescription (in tablets) and should be used under his supervision. Injection treatment is carried out in a hospital setting during exacerbation of coronary heart disease and CHF, tablets are prescribed on an ongoing basis in minimally effective doses, since the drug has a toxic and narcotic-like effect.
The therapeutic effect consists of changing the strength and amplitude of myocardial contractions (gives the heart energy, supports it in ischemic conditions). The drug also has a vasodilatory (reduces congestion) and some diuretic effect, which helps relieve swelling and reduce the severity of respiratory failure, manifested as shortness of breath.
The danger of Digoxin and other cardiac glycosides is that, if overdosed, they can provoke cardiac arrhythmia caused by increased excitability of the myocardium.
In case of exacerbation of CHF, the drug is prescribed in the form of injections, selecting an individual dosage taking into account the severity of the condition and the patient's age. When the condition stabilizes, they switch to tablets.
Usually, the standard single dose of the drug is 0.25 mg. The frequency of administration can vary from 1 to 5 times a day at equal intervals. In the acute stage of CHF, the daily dose can reach 1.25 mg, when the condition stabilizes on a permanent basis, it is necessary to take a maintenance dose of 0.25 (less often 0.5) mg per day.
When prescribing the drug to children, the patient's weight is taken into account. An effective and safe dose is calculated as 0.05-0.08 mg per kg of body weight. But the drug is not prescribed constantly, but for 1-7 days.
The dosage of cardiac glycoside should be prescribed by a doctor, taking into account the patient's condition and age. At the same time, it is very dangerous to adjust the doses independently or take 2 drugs with such an effect at the same time.
"Digoxin" is not prescribed for unstable angina, severe cardiac arrhythmias, grade 2-3 AV heart block, cardiac tamponade, Adams-Stokes-Morgagni syndrome, isolated bicuspid valve stenosis and aortic stenosis, congenital heart anomaly called Wolff-Parkinson-White syndrome, hypertrophic obstructive cardiomyopathy, endo-, peri- and myocarditis, thoracic aortic aneurysm, hypercalcemia, hypokalemia and some other pathologies. The list of contraindications is quite large and includes syndromes with multiple manifestations, so the decision on the possibility of using this drug can only be made by a specialist.
Digoxin also has side effects. These include heart rhythm disturbances (as a result of an incorrectly selected dose and overdose), loss of appetite, nausea (often with vomiting), bowel disturbances, severe weakness and high fatigue, headaches, the appearance of "flies" before the eyes, a decrease in the level of platelets and blood clotting disorders, allergic reactions. Most often, the appearance of these and other symptoms is associated with taking large doses of the drug, less often with long-term therapy.
"Spironolactone" is a mineralocorticoid antagonist. It has a diuretic effect, promoting the excretion of sodium, chlorine and water, but retaining potassium, which is necessary for the normal functioning of the heart, since its conductive function is mainly based on this element. It helps relieve edema. It is used as an adjuvant in congestive heart failure.
In case of CHF, the drug is prescribed depending on the phase of the disease. In case of exacerbation, the drug can be prescribed both in the form of injections and in tablets at a dosage of 50-100 mg per day. When the condition stabilizes, a maintenance dose of 25-50 mg is prescribed for a long time. If the balance of potassium and sodium is disturbed towards a decrease in the former, the dose can be increased until a normal concentration of trace elements is established.
In pediatrics, the effective dosage is calculated based on a ratio of 1-3 mg of spironolactone per kilogram of the patient's body weight.
As we can see, here too, the selection of the recommended dose is individual, as is the case with the prescription of many other drugs used in cardiology.
Contraindications to the use of a diuretic may be: excess potassium or low sodium levels in the body, pathology associated with the absence of urination (anuria), severe kidney disease with impaired performance. The drug is not prescribed to pregnant women and nursing mothers, as well as to those who have an intolerance to the components of the drug.
Caution should be exercised when using the drug in patients with AV heart block (may worsen), excess calcium (hypercalcemia), metabolic acidosis, diabetes mellitus, menstrual irregularities, and liver disease.
Taking the drug may cause headaches, drowsiness, loss of balance and coordination of movements (ataxia), enlargement of the mammary glands in men (gynecomastia) and impotence, changes in the nature of menstruation, coarsening of the voice and excessive hair growth in women (hirsutism), pain in the epigastrium and gastrointestinal disorders, intestinal colic, kidney dysfunction and mineral imbalance. Skin and allergic reactions are possible.
Side effects are usually observed when the required dose is exceeded. Edema may occur when the dosage is insufficient.
"Magnicor" is a drug that prevents the formation of blood clots, based on acetylsalicylic acid and magnesium hydroxide. One of the effective means of antithrombotic therapy prescribed for heart failure. It has an analgesic, anti-inflammatory, antiplatelet effect, affects the respiratory function. Magnesium hydroxide reduces the negative effect of acetylsalicylic acid on the gastrointestinal mucosa.
In case of endomyocardial fibroelastosis, the drug is prescribed for prophylactic purposes, therefore the minimum effective dose is adhered to - 75 mg, which corresponds to 1 tablet. In case of cardiac ischemia due to thrombus formation and subsequent narrowing of the lumen of the coronary vessels, the initial dose is 2 tablets, and the maintenance dose corresponds to the prophylactic dose.
Exceeding the recommended dosage significantly increases the risk of bleeding that is difficult to stop.
The dosages are indicated for adult patients due to the fact that the drug contains acetylsalicylic acid, the use of which at the age of under 15 years can have serious consequences.
The drug is not prescribed to patients of childhood and early adolescence, in case of intolerance to acetylsalicylic acid and other components of the drug, "aspirin" asthma (in history), acute erosive gastritis, peptic ulcer, hemorrhagic diathesis, severe liver and kidney diseases, in case of severe decompensated heart failure.
During pregnancy, Magnicor is prescribed only in cases of extreme necessity and only in the 1st-2nd trimester, taking into account the possible negative effect on the fetus and the course of pregnancy. In the 3rd trimester of pregnancy, such treatment is undesirable, since it contributes to a decrease in the contractility of the uterus (prolonged labor) and can cause severe bleeding. The fetus may have pulmonary hypertension and kidney dysfunction.
Side effects of the drug include symptoms from the gastrointestinal tract (dyspepsia, epigastric and abdominal pain, some risk of gastric bleeding with the development of iron deficiency anemia). Against the background of taking the drug, nosebleeds, bleeding gums and urinary system organs are possible,
Overdose may cause dizziness, fainting, and ringing in the ears. Allergic reactions are not uncommon, especially in the context of hypersensitivity to salicylates. However, anaphylaxis and respiratory failure are rare side effects.
The selection of drugs in complex therapy and recommended dosages should be strictly individual. Particular caution should be exercised in the treatment of pregnant women, nursing mothers, children and elderly patients.
Traditional medicine and homeopathy
Cardiac fibroelastosis is a serious and severe disease with a characteristic progressive course and virtually no chance of recovery. It is clear that effective treatment of such a disease with folk remedies is impossible. Traditional medicine recipes, which mainly come down to herbal treatment, can only be used as an auxiliary means and only with the permission of a doctor, so as not to complicate an already poor prognosis.
As for homeopathic remedies, their use is not prohibited, and can be part of a comprehensive treatment for heart failure. However, in this case, we are talking not so much about treatment as about preventing the progression of CHF.
The drugs should be prescribed by an experienced homeopath, and the question of the possibility of including them in complex therapy is within the competence of the attending physician.
What homeopathic medicines help to delay the progression of heart failure in fibroelastosis? In acute heart failure, homeopaths turn to the help of the following medicines: Arsenicum album, Antimonium tartaricum, Carbo vegetabilis, Acidum oxalicum. Despite the similarity of indications, when choosing an effective medicine, doctors rely on the external manifestations of ischemia in the form of cyanosis (its degree and prevalence) and the nature of the pain syndrome.
In case of CHF, the following may be included in the maintenance therapy: Lachesis and Nayu, Lycopus (in the initial stages of cardiac enlargement), Laurocerasus (for shortness of breath at rest), Latrodectus mactans (for valvular pathologies), hawthorn preparations (especially useful for endomyocardial lesions).
In case of strong heartbeat, the following may be prescribed for symptomatic treatment: Spigelia, Glonoinum (for tachycardia), Aurum metallicum (for hypertension).
To reduce the severity of shortness of breath, the following help: Grindelia, Spongia and Lahegis. To relieve heart pain, the following can be prescribed: Cactus, Cereus, Naya, Cuprum, to relieve anxiety against this background - Aconitum. In the development of cardiac asthma, the following are indicated: Digitalis, Laurocerasus, Lycopus.
Prevention
Prevention of acquired fibroelastosis of the heart and lungs consists of prevention and timely treatment of infectious and inflammatory diseases, especially when it comes to damage to vital organs. Effective treatment of the underlying disease helps prevent dangerous consequences, which include fibroelastosis. This is an excellent reason to take good care of your health and the health of future generations, the so-called work for a healthy future and longevity.
Forecast
The connective tissue changes associated with cardiac and pulmonary fibroelastosis are considered irreversible. Although some drugs can reduce the thickness of the endocardium somewhat with long-term therapy, they do not guarantee a cure. Although the condition is not always fatal, the prognosis is still relatively poor. The 4-year survival rate is 77%. [ 14 ]
The worst prognosis, as we have already mentioned, is with the congenital form of cardiac fibroelastosis, the manifestations of heart failure in which are visible already in the first weeks and months of the child's life. Only a heart transplant can save the baby, which in itself is a risky operation in such an early period, and it must be done before 2 years. Such children usually do not live longer.
Other operations only allow to avoid the early death of the child (and not always), but cannot completely cure him from heart failure. Death occurs with decompensation and development of respiratory failure.
The prognosis for pulmonary fibroelastosis depends on the characteristics of the disease. If symptoms develop rapidly, the chances are extremely small. If the disease progresses gradually, the patient can live for about 10-20 years, until respiratory failure occurs due to changes in the alveoli of the lungs.
Many difficult-to-treat pathologies can be avoided if preventive measures are taken. In the case of cardiac fibroelastosis, this is, first of all, the prevention of those factors that can affect the development of the heart and circulatory system of the fetus (with the exception of hereditary predisposition and mutations, against which doctors are powerless). If they cannot be avoided, early diagnostics helps to identify the pathology at a stage when termination of pregnancy is possible, which in this situation is considered humane.

