
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
External hemorrhoids in women and men
Medical expert of the article
Last reviewed: 04.07.2025
Hemorrhoids are a common condition that can cause symptoms ranging from minimal discomfort or inconvenience to excruciating pain and significant psychosocial consequences. [ 1 ]
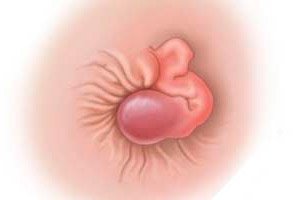
When varicose veins of the anal outlet and rectum occur, with the formation of tortuous formations - nodes - then they talk about such a disease as external hemorrhoids. Unlike the internal type, external pathology develops in the transition zone of the anus into the rectum, and not in its depth.
The earlier you start treatment, the faster and easier you can get rid of suffering. If you try to treat the problem yourself, or ignore it altogether, the disease will become chronic and will remind you of itself with regular exacerbations of the process. At the same time, an exacerbation at a late stage is no longer treated with medication: you have to resort to the help of a surgeon. Therefore, it is strongly recommended not to postpone a visit to the doctor.
Epidemiology
People with hemorrhoids and those who mistakenly believed they had hemorrhoids tended to self-medicate rather than seek proper medical care. [ 2 ] According to Google's annual survey in 2012 (Google Zeitgeist), hemorrhoids were the most common health problem in the United States, ahead of gastroesophageal reflux disease and sexually transmitted diseases. Unfortunately, the quality of hemorrhoid treatment information on the Internet is now very variable, with nearly 50% of websites being of poor quality. [ 3 ] Therefore, clinicians should advise and treat patients with hemorrhoids using evidence-based medicine and standards of care.
Almost any of us can get external hemorrhoids: those who sit often and for a long time, for example, in an office or behind the wheel of a car, are most susceptible to this disease. People with bad habits and poor nutrition, who suffer from constipation and other digestive disorders, are also “targeted”. Heavy physical work is another prerequisite for the problem, so often loaders and even weightlifters become patients of proctologists.
Hemorrhoids are a common anorectal disorder affecting millions of people in the United States and are the most common cause of rectal bleeding. Hemorrhoids are thought to be equally common in both men and women. They are rare before age 20, and the incidence peaks between the ages of 45 and 65. The prevalence of hemorrhoids in pregnant women varies up to 35%. [ 4 ]
About 10% of patients in the proctology office seek medical attention specifically because of external hemorrhoids.
Causes external hemorrhoids
Experts are still silent about the exact causes of external hemorrhoids, but there are basic theories about this. So, most often the reasons can be as follows:
- daily insufficient physical activity, prolonged standing or sitting, leading to blood stagnation in the pelvic area;
- excessive physical activity associated with lifting and carrying heavy objects, creating increased intra-abdominal pressure;
- problems with defecation, stool instability;
- eating disorders, including alcohol abuse and spicy food;
- deterioration of blood flow in the pelvic area, which may be associated with overheating or hypothermia of the specified area;
- the period of pregnancy, natural childbirth, when there is a strong increase in intra-abdominal pressure against the background of impaired venous outflow;
- excess weight, localized mainly in the waist area;
- regular anal intercourse;
- pathologies that are accompanied by a violation of venous outflow (diseases of the liver, bladder, prostate gland, intestines, as well as tumors in the pelvic area);
- congenital anomalies of connective tissue, venous vessels.
Sometimes it may seem that there are no predisposing factors – and yet external hemorrhoids have appeared. This happens if a person is subject to constant stress or suffers from emotional instability, which leads to a prolonged spasm of the smooth muscle fibers of the vascular walls. This factor is often not given special importance, and completely in vain. In addition, there are hereditary reasons: if one of the parents suffers from external hemorrhoids, then the risk of developing the disease increases in children.
Risk factors
Factors that contribute to the development of external hemorrhoids are conventionally divided into two categories:
- Internal factors include the following:
- congenital vascular defects;
- systemic disorders affecting the vascular network (for example, vasculitis);
- digestive disorders, which are often accompanied by constipation, hard stool, etc.;
- aging, obesity, abdominal obesity, depressive mood and pregnancy; [ 5 ]
- other causes that contribute to the creation of high intra-abdominal pressure. [ 6 ]
- External factors include:
- traumatic injuries to the anal area (for example, during childbirth, anal sex, etc.);
- regular lifting and carrying of heavy objects;
- physical inactivity, prolonged sitting position, lack of physical activity.
- Certain foods and lifestyle factors, including low-fiber diets, spicy foods, and alcohol consumption, have been reported to be associated with the development of hemorrhoids and exacerbation of acute hemorrhoid symptoms.[ 7 ]
Pathogenesis
The exact pathophysiology of symptomatic hemorrhoids is poorly understood. Previous theories of hemorrhoids as varicose veins are now obsolete - as shown by the studies of Goenka et al. Patients with portal hypertension and varicose veins do not have an increased incidence of hemorrhoids. [ 8 ]
The sliding anal mucosa theory is now more widely accepted, which suggests that hemorrhoids occur when the supporting tissues of the anal nodes deteriorate. Age and strenuous physical activity, straining during bowel movements, and prolonged sitting are thought to contribute to this process. Therefore, hemorrhoids are a pathological term to describe the abnormal downward displacement of the anal nodes, causing varicose veins. [ 9 ]
On histopathological examination, changes observed in anal nodes include abnormal venous dilation, vascular thrombosis, degenerative process in collagen fibers and fibroelastic tissues, and deformation and rupture of the anal subepithelial muscle. In severe cases, a marked inflammatory reaction involving the vascular wall and surrounding connective tissue has been associated with mucosal ulceration, ischemia, and thrombosis.[ 10 ]
External hemorrhoids are accompanied by the expansion of hemorrhoidal nodes formed in the lower venous plexus. Such nodes are located directly at the anus. Since the inflammatory process occurs not in the depths, but outside the intestine, then in most cases the problem can be seen with the naked eye.
The final segment of the intestinal tract, which ends the large intestine, is called the rectum. Its beginning roughly corresponds to the level of the third sacral vertebra, and the final element is the anus.
Five arterial vessels are responsible for the blood supply to this area, one of which is called the "hemorrhoidal artery." Blood flows out through an extensive venous network, which is located in the rectal submucosal layer.
With weak connective tissue and vascular walls, blood flow is present, but outflow is disrupted, which leads to swelling of the veins, overflow of blood in the cavernous bodies. In some cases, the "culprits" are mechanical factors that lead to stretching and weakening of the rectal muscles, which contributes to the movement of hemorrhoids to the anal area and prolapse from it.
Symptoms external hemorrhoids
Overall, 40% of people with hemorrhoids are asymptomatic.[ 11 ]
External hemorrhoids do not appear immediately: their development with increasing symptoms occurs gradually. A person does not immediately notice the disorder, and only over time begins to pay attention to uncomfortable, pulling, itching or painful sensations in the anus, especially when sitting for a long time or after defecation.
The first signs can be noticed upon detailed examination of the anal area: it is often swollen, with noticeable bulging veins. Sometimes discharge is detected - for example, blood spots appear on toilet paper or underwear. If at least one of the above signs is present, then it is necessary to go to see a doctor.
External hemorrhoids are accompanied by the expansion of hemorrhoidal venous vessels: nodes are formed from the lower plexus of veins, which are located in close proximity to the anus. Since the inflammatory process is not present in the rectum, but outside it, the main role in making a diagnosis is played by a visual examination of the problem and a digital (rectal) examination.
Bleeding does not become a typical symptom, but external nodular formations are often inflamed and damaged, which can be seen with the naked eye.
It is important to take into account that external hemorrhoids rarely occur on their own. The problem is often combined, internal-external, with deformation of the cavernous bodies of the rectum and the subcutaneous venous plexus of the anal area.
Psychosomatics in hemorrhoids
Psychological problems are rarely considered by doctors as the main causes of the development of such a disease as hemorrhoids. However, it has been scientifically proven that prolonged stress, anxiety, and fears can cause serious health problems.
A state of physical discomfort should always alert both the patient and the doctor. If you review your own attitude to problems and life in general in a timely manner, you can significantly improve your health and prevent the development of many diseases. Experts point out that psychosomatics in hemorrhoids is not difficult: it is only important to pay attention to certain aspects of life.
Scientists explain the appearance of external hemorrhoids by people's unwillingness to admit their own mistakes and errors, to point out the problems of others, while not noticing their own. The inflammatory process is a consequence of individual insecurity, hemorrhoidal bleeding is the result of angry feelings associated with the impossibility of implementing one's plans, and dilated venous nodes are the result of constant procrastination, lack of organization and regular putting off of things for "later".
In addition, excessive "fixation" on something leads to energy and then to blood stagnation. Additional "provocateurs" are constant tension, lack of satisfaction in everything, suppression of one's own emotional impulses.
External cone with hemorrhoids
What is a lump in external hemorrhoids? It is a dense painful nodule (often one or two) in the anal area, quite sensitive to touch, and especially sensitive to pressure. Such nodes are located around the anus, and even deep in the anal canal. From patients, you can hear different terms regarding a hemorrhoidal nodule - it is not only a "lump", but also a "tumor", "sealing", "prolapse".
Why does the appearance of a lump cause pain? Blood clots inside venous dilatations stretch the walls of the vessel, affecting the nerve endings, which causes pain.
Patients come to the doctor mainly with complaints of a foreign body sensation and pain. Unpleasant symptoms intensify during defecation, physical activity, and prolonged sitting. The "bumps" may have a reddish or bluish tint, depending on the stage of the disease process. When anal fissures appear, bleeding is noted.
External hemorrhoids in women
External manifestations of hemorrhoids can bother any person, regardless of gender. But the course of the disease in men and women is slightly different. What's the matter?
Hormonal cyclical fluctuations associated with periods of menstruation and ovulation can provoke an exacerbation of chronic external hemorrhoids in women. It is with such fluctuations that discomfort, a feeling of heaviness, and pain in the anus are associated. These symptoms are to some extent natural and easily explained: with the beginning of a new monthly cycle, blood flows intensely to the pelvic organs, the veins overflow, which becomes a factor in the exacerbation of the disease.
To reduce the likelihood of relapse, a few days before the onset of menstruation, you should stop eating salt, sugar, and hot spices. If there is an increased risk of exacerbation due to the urge to defecate, it is recommended to insert a rectal suppository with belladonna into the rectum, which will relieve the spasm, ease the load, and relax the rectal sphincter.
External hemorrhoids during pregnancy occur most frequently in women, especially in the third trimester. [ 12 ] The growing uterus makes it difficult to empty the bowels, and the altered hormonal background contributes to the appearance of constipation. A large amount of feces accumulates in the intestines, squeezing the blood vessels and impairing the outflow of blood from the veins. Stagnation occurs, contributing to the expansion of the vascular walls.
Natural childbirth is another provoking factor for the exacerbation of hemorrhoids, because heavy pushing is accompanied by colossal tension of the abdominal muscles with a violation of vascular blood circulation. As a result - dilated venous nodes, pain and swelling.
External hemorrhoids in men
In the representatives of the strong half of humanity, external hemorrhoids are often combined with other pathologies - for example, with internal hemorrhoids, prostatitis, etc. And the male problem appears under the influence of such factors:
- predominantly sedentary work (drivers, programmers, etc.);
- alcohol and nicotine abuse (the digestive system is disrupted, chronic intoxication occurs);
- widespread nutritional disorders (fast food, processed foods, chips, snacks, dry snacks;
- obesity, extra pounds in the abdominal area;
- lifting and carrying heavy objects (causes tension and even spasm of the annular muscles of the anus, as well as an increase in intra-abdominal pressure).
It is typical that in most cases men turn to the doctor about a delicate problem – hemorrhoids, already in advanced cases, because they endure and “delay” a visit to the doctor as long as possible. But in the later stages the risk of developing adverse effects increases significantly, and the disease is more difficult to treat, often requiring surgery.
In order for the problem not to bother and not to darken the existence of a man, the specialist recommends to regularly visit a doctor for a preventive examination, eat right, refuse all sorts of "harmful" and alcoholic drinks, do feasible physical work, avoiding both excessive loads and sedentary pastime. It is necessary to maintain intimate hygiene and not be embarrassed to contact a doctor at the first signs of discomfort.
Stages
- Stage 1 of external hemorrhoids rarely causes concern on the part of the patient, since the signs of the disease are not yet sufficiently expressed. Minor discomfort appears against the background of intestinal disorders, after physical overload, prolonged sitting, or after a sharp temperature change. Minor itching and burning after defecation goes away on its own and relatively quickly. This stage is easier to treat than others, but at this stage, people consult doctors the least.
- Stage 2 of external hemorrhoids is characterized by an increase in the dilated nodes, thinning of their walls, and the formation of cracks. After physical overload, strong straining, bleeding and slight soreness may be observed. A long stay in a sitting position is accompanied by pain.
- Stage 3 of external hemorrhoids is characterized by dystrophic changes and weakness of the vessel walls. The patient complains of constant discomfort, itching, pain, decreased sphincter tone. Sitting and working becomes physically impossible.
- Stage 4: Hemorrhoids that are always located outside the anus and can no longer be pushed back inside. Usually, a small amount of anal mucus comes out of the anus. This stage is also known as rectal prolapse. [ 13 ]
Forms
In general, hemorrhoids can be not only external, but also internal, and mixed (combined internal and external). The external variant is distinguished by the fact that hemorrhoidal expansions are formed in the lower venous plexus and are located right next to the anus. External hemorrhoids are located below the dentate line and drain through the lower rectal veins into the genital vessels, and then into the internal iliac vein. These vessels are covered with anoderm, which consists of squamous epithelium. [ 14 ]
A distinction is also made between acute and chronic courses of the disease.
Acute external hemorrhoids occur suddenly, symptoms increase in a short period of time. The inflammatory process quickly spreads to nearby tissues, severe pain is disturbing.
Chronic external hemorrhoids are characterized by a gradual increase in symptoms with periodic exacerbations. The disease lasts for a long time, for many months and even years.
An exacerbation of external hemorrhoids makes itself known by bleeding, pain and severe discomfort. The nodes increase in size, there is a sharp pain when touched. During periods of symptomatic relief, the patient complains of almost nothing, but soon the disease makes itself known again.
Complications and consequences
If you do not seek medical help in time, external hemorrhoids can be complicated by more painful conditions:
- bleeding, hemorrhage - both after the act of defecation, and against the background of a crack, or even without a specific reason;
- prolapse of an enlarged venous node - more often observed in the chronic course of the disease, against the background of prolonged constipation;
- mechanical injuries to the inflamed hanging node;
- thrombosis of the dilated vein, which is accompanied by swelling, severe pain, inflammatory and necrotic processes. [ 15 ]
Constant mechanical damage to dilated veins can cause malignant tissue degeneration: this occurs in approximately 10% of cases.
However, most often the disease is complicated by acute hemorrhoidal thrombosis or the development of posthemorrhagic anemia. To prevent such adverse effects, it is recommended to periodically take phlebotonics, follow a diet and eliminate bad habits.
A serious consequence of advanced forms of hemorrhoids can be a necrotic process in the tissues of the hemorrhoidal expanded segment. The beginning of such a process is characterized by blackening of the nodes, the pain may dull or disappear altogether. This problem is eliminated only in a hospital: the help of a surgeon is required to remove areas of necrosis.
How many days does external hemorrhoids last? The healing period depends on several factors - first of all, on what stage the disease is at. Therefore, there can be no clear answer to this question. For example, the first stage can be cured within a week. But at stage II or III, the treatment is definitely longer: from several weeks or more. If surgical intervention is used, then the healing period here depends on how invasive and traumatic the intervention was.
What to do if external hemorrhoids do not go away? The disease itself cannot go away: it needs to be treated. Therefore, it is necessary to see a doctor, and there is nothing to be embarrassed or afraid of. The sooner medical assistance follows, the better the prognosis, and the sooner the long-awaited relief will come. We must not forget that advanced external hemorrhoids are much more difficult to treat: at a late stage, drug therapy is usually already ineffective, so surgical removal of dilated venous nodes is required.
External hemorrhoids hurt during an exacerbation, or against the background of the appearance of an anal fissure, which behind the external hemorrhoidal tubercles can become completely invisible and is discovered only during a diagnostic examination.
But blood and bleeding with external hemorrhoids are rare. Although, if there is one, another complication may arise: posthemorrhagic anemia. Regular bleeding imperceptibly leads to a fairly significant loss of blood, which can later be noticed when examining the results of laboratory tests. In turn, anemia causes other ailments: the patient feels constant weakness, dizziness, nausea, dark circles under the eyes, sleep and appetite are disturbed.
Thrombosis in external hemorrhoids is considered a formidable complication, which is accompanied by severe pain, and if no help is provided, tissue necrosis processes may begin. Prevention of this problem can be the use of venotonics and anticoagulants, correction of the diet and drinking regime. [ 16 ]
Can a dilated segment of a venous vessel burst? It can, however, it rarely happens when external hemorrhoids burst – more often such a complication occurs with internal vascular damage. The likelihood of the problem increases if the vein is thrombosed or overflows with blood – for example, this happens with severe and prolonged constipation.
But inflammation of external hemorrhoids can develop into acute paraproctitis - this is a painful process affecting the pararectal tissue. The pathology is characterized by signs of pararectal suppuration: swelling, pain, central fluctuation, an increase in temperature to subfebrile values. Then signs of general intoxication appear. Medical assistance in such a situation should be urgent.
When such an unpleasant consequence as perianal pruritic dermatitis develops, the patient notes that external hemorrhoids itch. This does not happen often, and the cause is usually improper perineal hygiene, failure to observe the defecation regime. If the itching is persistent, the doctor may recommend the use of antipruritic agents, as well as ointments with glucocorticoid components. [ 17 ], [ 18 ], [ 19 ]
Diagnostics external hemorrhoids
Standard diagnostics by a proctologist involves collecting anamnesis (questioning the patient) and digital examination. If a digital procedure is not possible – for example, in case of severe pain – then treatment is prescribed immediately, and diagnostics are continued after the painful symptoms disappear. [ 20 ]
In general, diagnosis of external hemorrhoids includes:
- Digital palpation determines the type of disease.
- Instrumental diagnostics:
- anoscopy, which is the insertion of a special device into the rectal cavity to a depth of 140 mm;
- Rectoscopy involves the insertion of a rectoscope equipped with an optical system and displaying an image on a computer monitor;
- Irrigoscopy involves taking X-rays using contrast.
- Laboratory tests:
- stool analysis (coprogram, stool for occult blood);
- General clinical blood and urine tests.
Differential diagnosis
Differential diagnostics are performed with anal fissures, malignant or benign rectal neoplasms, ulcerative colitis, traumatic injury, solitary ulcerative lesion, Crohn's disease, [ 21 ] with rectal prolapse, submucous hemangioma. In the presence of severe pain, it is important to differentiate with acute thrombosis of venous dilatations, with exacerbation of paraproctitis, anal tumor processes, proctalgia, Crohn's disease. In case of anal itching, it is necessary to exclude insufficient function of the anal sphincter, villous rectal tumor formation, chronic paraproctitis, diabetes mellitus, fungal infection, helminthiasis, perianal condyloma. Sometimes such symptoms are present with banal non-observance of hygiene of the perineum and genitals.
Contrary to previous studies, the incidence of hemorrhoids in patients with portal hypertension does not differ from the general population.[ 22 ] Varicose veins, which are the result of porto-systemic communication through hemorrhoidal veins, are commonly found in patients with portal hypertension. However, bleeding from rectal varices is rare, accounting for less than 1% of massive bleeding in portal hypertension.[ 23 ]
How to understand whether hemorrhoids are external or internal?
External hemorrhoids are nodular dilations of the venous vessels located near the anus. In most cases, the problem is visible to the naked eye, because the inflammatory process occurs outside, not in the rectum. But bleeding during the external process does not always bother: the main symptom is still pain. [ 24 ]
Internal pathology is localized in the submucous tissue of the rectum. It is difficult to see such hemorrhoids, but you can notice the presence of blood - for example, it can be blood in the feces, or red spots on toilet paper or underwear. At a late stage of the disease, the enlarged nodes slip out of the anus.
Internal and external hemorrhoids are often found together, in combination with each other: in this situation, they talk about a combined form of the disease. This pathology is characterized by deformation of the cavernous bodies of the rectum and the subcutaneous venous network of the anal area.
Treatment external hemorrhoids
Treatment for hemorrhoids is prescribed in a complex, since it is impossible to cure the disease with any one medication or procedure. In the early stages, conservative methods are used, which include changes in nutrition and lifestyle, as well as the use of systemic drugs and external agents (ointments, creams, etc.).
For symptomatic treatment, topical preparations containing various local anesthetics, corticosteroids, or anti-inflammatory active agents are available. Notable topical preparations include 0.2% glyceryl trinitrate, which has been studied for the relief of grade I or II hemorrhoids.[ 25 ] Patients also commonly self-medicate with preparations containing phenylephrine, mineral oil, and shark liver oil (which has vasoconstrictor and protective properties), which provide temporary relief of acute hemorrhoid symptoms such as bleeding and pain with defecation.[ 26 ] Topical corticosteroids in creams or ointments are often used, but their effectiveness remains unproven.
Oral preparations containing flavonoids are the most common phlebotonic agent used to treat hemorrhoids. Apparently, flavonoids can increase vascular tone, decrease venous capacitance, decrease capillary permeability, improve lymphatic drainage, and have anti-inflammatory effects. [ 27 ] A large meta-analysis of phlebotonic use in hemorrhoids in 2012 found that phlebotonics had a significant beneficial effect on bleeding, itching, discharge, and overall improvement in symptoms. Phlebotonics also relieved symptoms after hemorrhoidectomy. [ 28 ]
Oral calcium dobesilate is another venotonic drug commonly used in diabetic retinopathy and chronic venous insufficiency, as well as in the treatment of acute hemorrhoid symptoms.[ 29 ] Calcium dobesilate has been shown to reduce capillary permeability, inhibit platelet aggregation, and improve blood viscosity; resulting in a reduction in tissue edema.[ 30 ] A clinical trial in the treatment of hemorrhoids found that calcium dobesilate in combination with fiber supplementation provided effective symptomatic relief from acute bleeding, and this was associated with a significant reduction in the inflammatory response in hemorrhoids.[ 31 ]
Except in cases of thrombosis, both internal and external hemorrhoids respond easily to conservative drug therapy.
Surgical treatment is considered when conventional measures are no longer effective. For patients with thrombosed external hemorrhoids, surgical exploration and intervention within 72 hours of thrombosis can provide significant relief, as pain and swelling peak at 48 hours. [ 32 ] However, surgery is usually not considered after 48-72 hours, as the thrombus is organized and symptoms are reduced. At this point, the pain from hemorrhoid excision will exceed the pain from the thrombosis itself.
In addition to anti-inflammatory, analgesic, antibacterial, venotonic and anticoagulant drugs, special attention is paid to diet:
- you should consume at least 500 g of plant foods daily;
- It is useful to add bran to your diet;
- When choosing bread, you need to choose products made from wholemeal flour;
- It is important to exclude hot spices, fried and smoked foods, alcoholic beverages from the menu, and also to give up smoking;
- It is not recommended to suppress the urge to defecate.
In a meta-analysis of seven randomized trials comparing fiber with other fibers, fiber supplementation (7–20 g/day) reduced the risk of symptoms and bleeding by 50% in hemorrhoids. However, fiber intake did not reduce prolapse symptoms, pain, or itching.[ 33 ]
Thus, fiber supplements are considered effective in treating hemorrhoids; however, it may take up to 6 weeks to see significant improvement in symptoms. [ 34 ] Because fiber supplements are safe and inexpensive, they remain an integral part of both initial treatment and a treatment regimen following other hemorrhoid treatments.
In addition, special attention is paid to physical activity.
Sports for external hemorrhoids
Hemorrhoids and sports are often incompatible concepts, especially when it comes to professional sports. However, some types of physical activity are even welcomed: the main thing is not to forget that excessive load will only worsen the course of the disease.
Types of physical exercise permitted for external hemorrhoids should help normalize blood flow in the pelvic area, and the load on the already affected veins should be moderate. Ideally, patients should engage in swimming, sports or Nordic walking, and practice yoga.
As for other sports, you should get recommendations from your doctor, as they may vary in each specific case. In general, the following principles are important:
- during periods of exacerbation, any stress should be excluded altogether;
- You cannot play sports immediately after surgery to remove hemorrhoids;
- You cannot self-medicate or ignore your doctor’s orders and advice.
The following sports are considered extremely undesirable and even unsafe for patients with external hemorrhoids:
- strength sports, powerlifting;
- weightlifting, bodybuilding;
- cycling, horse riding;
- all kinds of martial arts.
Exercises for external hemorrhoids
There are a number of physical activity options that are permitted and even recommended for people suffering from external hemorrhoids. For example, to stimulate blood flow and relieve the load on the anal area, it is recommended to do the following exercises:
- The well-known “birch”: lie on your back, raise your legs together with your pelvis into a vertical position, hold for a few minutes, and return to the starting position.
- "Scissors": lie on your back, raise your straight legs at a slight angle from the floor, and make crossing movements like cutting with scissors.
- “Half bridge”: lying on your back, lift your pelvis up as much as possible, squeezing your gluteal muscles (without using your hands for support).
Squats are not recommended for hemorrhoids, as are regular “press-ups,” since these exercises create high pressure on hemorrhoidal veins. But race walking is a great way to keep yourself in shape without harming your health. Exercises should begin approximately two hours after a meal, choosing a comfortable speed for yourself.
There is another simple and unnoticeable exercise that can be performed for therapeutic and preventive purposes. Its essence is as follows: strain the muscles of the anus, as if drawing it deeper. Fix this position for a few seconds, then relax. Repeat up to ten times. This exercise, unnoticeable to others, helps eliminate blood stagnation in the rectum area.
Prevention
The best treatment is prevention. In terms of prevention, special attention should be paid to nutrition and lifestyle. [ 35 ] The main points should be remembered and always followed:
- Particularly desirable products for those prone to hemorrhoids include fruits and vegetables, greens and berries, bran, fermented milk products (kefir or fermented baked milk, natural yogurt, sour milk and cottage cheese), as well as cereals - in particular, buckwheat, oatmeal, barley groats.
- You should not drink whole milk, alcoholic beverages, eat sausages and smoked meats, sweets and pastries, spicy, fatty and overly salty foods.
- If you experience any discomfort in the anal area, you should not take any action on your own; it is better to see a doctor immediately.
- After each act of defecation, it is advisable to wash yourself or wipe the anus with a damp cloth.
- Constipation should not be allowed to occur, but relying on laxatives is also not recommended. Both constipation and frequent loose stools are dangerous for the health of the rectum.
- If you are prone to external hemorrhoids, it is not advisable to visit a sauna, take a hot bath, or sit on hot or cold surfaces.
- Excessive straining during bowel movements should be avoided.
- It is important to be active, walk often, and lift less weights.
Forecast
The possibility of prognosis for external hemorrhoids is determined by the neglect of the disease, the timeliness of seeking medical help. Prescribed drug therapy will not bring results if it is not combined with diet and lifestyle correction, with the establishment of physical activity.
Unfortunately, for most patients, conservative treatment can only "muffle" painful symptoms, but it is not able to completely cure external hemorrhoids. Therefore, it is often necessary to use surgical methods of influence - minimally invasive and traditional.

