
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
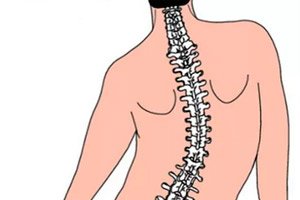
Dysplastic scoliosis
Medical expert of the article
Last reviewed: 12.07.2025
Among the scoliosis-related deforming dorsopathies with the code M40-M43 in the International Classification of Diseases (ICD-10), dysplastic scoliosis is absent. Although there is a code M41.8 - other forms of scoliosis, one of which is scoliosis caused by dysplasia, that is, an anomaly in the development of the structures of the lumbosacral spine during embryogenesis.
Epidemiology
As noted by clinical statistics, childhood idiopathic scoliosis accounts for 1.7%, with most cases occurring at 13 and 14 years of age, and small scoliotic curves (10–19 degrees) were the most common (prevalence 1.5%). [ 1 ] The female-to-male ratio ranges from 1.5:1 to 3:1 and increases significantly with age. In particular, the prevalence of curves with higher Cobb angles is significantly higher in girls than in boys: the female-to-male ratio increases from 1.4:1 for curves from 10° to 20° to 7.2:1 for curves > 40°. [ 2 ]
In 90-95% of cases, right-sided dysplastic thoracic scoliosis is observed, in 5-10% of cases – idiopathic or dysplastic left-sided lumbar scoliosis (right-sided lumbar scoliosis develops rarely).
According to the Scoliosis Research Society, juvenile scoliosis accounts for 12-25% of cases, and is diagnosed more often in girls than in boys. [ 3 ] The typical location is the thoracic spine; up to about 10 years of age, the pathology progresses slowly, but has a higher probability of developing severe deformity that is not amenable to conservative treatment.
The most common type of dysplastic scoliosis is in adolescence, with a general incidence in the population of up to 2% (with a predominance of girls).
Moreover, dysplastic thoracolumbar scoliosis is observed four times more often than lumbar scoliosis.
Causes dysplastic scoliosis
Western and many domestic specialists in the field of orthopedics and spinal pathology do not single out dysplastic scoliosis separately: it is classified as an idiopathic form, since the causes of many congenital anomalies in the development of spinal structures have not yet been established. Idiopathic scoliosis is, in a sense, a diagnosis of exclusion. However, idiopathic scoliosis is currently the most common type of spinal deformity. [ 4 ] It should be noted that at least 80% of scoliosis in children is idiopathic. [ 5 ] But as a final diagnosis, it is determined after excluding genetically determined generalized syndromes accompanied by congenital scoliosis.
Some experts associate the etiology of idiopathic or dysplastic scoliosis with genetics, since the spine is formed before birth, and this pathology is observed in the family: according to the Scoloosis Research Society, in almost a third of patients. And there is an opinion that scoliosis caused by dysplasia is a multigenic dominant condition with multivariate gene expression (but specific genes have not yet been identified). [ 6 ]
Other researchers, analyzing and systematizing clinical cases, see the causes of this pathology in metabolic disorders or teratogenic effects of various etiologies.
However, congenital morphological disorders of the spine (primarily in the lumbosacral region), which can lead to its three-dimensional deformation, are considered to be:
- spinal hernias, in particular meningocele;
- non-fusion of the posterior vertebral arches - spina bifida;
- spondylolysis – dysplasia of the vertebral arches with interarticular diastasis (gap);
- anomalies of the spinous processes of the vertebrae;
- developmental defect (in the form of a wedge) of the bodies of the first sacral vertebra (S1) and the fifth lumbar (L5);
- inferiority of the connective tissue structures of the spine in the form of dysplasia of the intervertebral discs.
When diagnosing dysplastic lumbar scoliosis, patients may be diagnosed with ontogenetic disorders of spinal segmentation such as lumbarization and sacralization.
During lumbarization (lumbar vertebrae – lumbar spine) in the embryonic period, the so-called transitional lumbosacral vertebra is formed, then the S1 vertebra does not merge with the sacrum and remains mobile (sometimes it is designated L6).
Sacralization (os sacrum – sacrum) is a condition in which during the period of intrauterine skeletal formation the transverse spinous process of the L5 vertebra fuses with the sacrum or ilium, forming a partial pathological synostosis. According to statistics, these anomalies are found in one baby out of 3.3-3.5 thousand newborns.
Risk factors
The risk of developing dysplastic scoliosis increases in the presence of the following factors:
- scoliotic deformity of the spine in the family history;
- intrauterine developmental disorders in the early stages of pregnancy (during the first 4-5 weeks), causing congenital defects in the structures of the spine;
- age and gender. This refers to the immaturity of the spine in children during their period of rapid growth: from infancy to three years and after nine years, as well as with the onset of puberty - the sexual maturation of adolescents, especially girls, in whom the disease often progresses and requires surgical intervention.
Pathogenesis
Explaining the pathogenesis of deformation of the spinal column in the frontal plane, which is accompanied by simultaneous twisting (torsion) of the vertebrae, orthopedists and vertebrologists note not only the anatomical and biomechanical features of the spine, but also the factors of its normal or abnormal formation at the initial stage of the period of intrauterine development - during somitogenesis.
Experts claim that almost all congenital defects of the spine structures of the future child are "laid down" before the end of the first month of pregnancy, when the cellular restructuring of the cytoskeleton occurs. And they are associated with disturbances in the processes of formation and distribution of somites - paired segments of mesodermal tissue.
As for the pathophysiology of spinal deformity in dysplastic scoliosis, for example, congenital morphological abnormalities of the vertebral bodies – the formation of so-called wedge-shaped vertebrae or semi-vertebrae – cause asymmetry and compensatory changes (curvature) of adjacent vertebrae. As the child grows, ossification zones (ossification nuclei) form on the surfaces of the vertebral joints, and the formation of spongy bone tissue instead of cartilaginous tissue leads to the fixation of the spinal column deformation.
In case of defects of the spinous processes, the surfaces of the vertebral joints are displaced (in case of their underdevelopment), or – when the processes are hypertrophied – their articulation is disrupted. The stability of the spinal column is also lost due to dysplasia of the intervertebral discs.
Symptoms dysplastic scoliosis
What are the clinical symptoms of dysplastic scoliosis? They depend on the localization of the pathological process and the degree of frontal deviation of the spinal column.
According to localization, the following are distinguished:
- dysplastic thoracic scoliosis – with the highest point of curvature of the spine at the level of the thoracic vertebrae T5-T9;
- thoracolumbar scoliosis – in most cases S-shaped, that is, with two oppositely directed arcs of curvature in the frontal plane; the apex of the lumbar arc is noted at the level of the first lumbar vertebra (LI), and the contralateral thoracic – in the region of the T8-T11 vertebrae;
- lumbar scoliosis – with the apical point of curvature in the area of the lumbar vertebra L2 or L3.
Approximately one quarter of patients with adolescent idiopathic scoliosis (AIS) experience back pain. [ 7 ] Symptoms may also include paresthesia and paresis of the extremities, toe deformities, loss of tendon reflexes, blood pressure variability, pollakuria, and nocturnal enuresis. [ 8 ]
See also – Symptoms of scoliosis.
Stages
According to the accepted method, specialists determine the magnitude of the curvature arc – the degree of deviation (Cobb angle) based on an X-ray of the spine:
- dysplastic scoliosis of the 1st degree corresponds to a curvature angle of up to 10°;
- Grade 2 is diagnosed when the Cobb angle is in the range of 10-25°;
- 3 degrees means that the deviation of the spine in the frontal plane is 25-50°.
Higher Cobb angle values provide grounds for declaring grade 4 scoliosis.
At the 1st degree of curvature, both the first signs and pronounced symptoms may be absent. The progression of the pathology begins to manifest itself in posture disorders with a distorted waist line and different heights of the shoulder blades and shoulders.
With lumbar scoliosis, there is a tilt of the pelvis, which is accompanied by a protrusion of the upper edge of the ilium, a feeling of shortening of one leg and limping.
With scoliosis of 3-4 degrees, pain may appear in the back, pelvic area, lower limbs. Rotation of the vertebrae with an increase in the angle of curvature leads to protruding ribs and the formation of a front or back hump.
Complications and consequences
Any scoliosis with a frontal deviation of the spine of more than 40° has negative consequences and gives complications, and this is not only a hump that disfigures the body. According to the study, scoliosis progression was observed in 6.8% of students and 15.4% of girls with scoliosis of more than 10 degrees during the initial examination. In 20 percent of children with curves of 20 degrees during the initial examination, there was no progression. Spontaneous improvement of the curve occurred in 3% and was more often observed on curves less than 11 degrees. Treatment was required for 2.75 children out of 1000 examined. [ 9 ]
Since the progression of curvature is related to growth potential, the younger the patient is in the initial stage of scoliosis, the greater the degree of deformation of the spinal column can be.
Thus, dysplastic thoracolumbar or lumbar scoliosis, which develops in children under 5 years of age, can disrupt intraorgan blood flow and adversely affect the cardiopulmonary, digestive and urinary systems. [ 10 ]
Diagnostics dysplastic scoliosis
Detailed information on the detection of this disease can be found in the article – Diagnosis of scoliosis.
Instrumental diagnostics is primarily carried out using radiography and spondylometry, as well as computed tomography of the spine.
Read also – Methods of examination of the spine
MRI of the brain and spinal cord may be required to rule out CNS disorders in patients under eight years of age with a spinal curvature angle greater than 20°.
Differential diagnosis
Differentiation of some diseases accompanied by spinal deformity is necessary. In addition, differential diagnostics is important to determine stable or minimally progressive scoliosis, which can be observed and corrected, and scoliosis with a large compensating lateral curvature and torsion of the vertebrae and a high risk of increasing the angle of curvature. In the second case, a referral to an orthopedic surgeon is necessary.
Who to contact?
Treatment dysplastic scoliosis
Methods and techniques for treating dysplastic scoliosis – including physiotherapy (various procedures, exercise therapy, massage) [ 11 ] – are described in detail in the publications:
In what cases surgical treatment is necessary to correct spinal deformity, [ 12 ] and how it is carried out is described in detail in the articles:
Prevention
Dysplastic scoliosis cannot be prevented, according to the Pediatric Orthopedic Society of North America.
However, early detection of deforming changes in the spine, i.e. prevention of severe curvatures, is possible through screening. Pediatric orthopedists should examine girls at 10 and 12 years of age, and boys should be checked once – at 13 or 14 years of age. [ 13 ]
Forecast
Once a diagnosis of dysplastic scoliosis has been made, the prognosis is related to the risk of progression of the deformity.
The determining factors are: the magnitude of the curvature at the time of diagnosis, the patient's future growth potential and his or her gender (since girls have a much higher risk of progression than boys).
The more severe the curvature of the spine and the greater the growth potential, the worse the prognosis. Growth potential is assessed by determining the stage of sexual development according to Tanner and the degree of ossification according to the Risser apophyseal test. [ 14 ]
Without treatment, dysplastic scoliosis of 1, 2 and 3 degrees in a teenager will progress by an average of 10-15° during life. And with a Cobb angle of more than 50°, its increase is 1° per year.

