
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Diagnosis of streptoderma in a child
Medical expert of the article
Last reviewed: 06.07.2025
In order to diagnose streptoderma in children, it is necessary to consult a doctor. This may be a local pediatrician, dermatologist, infectious disease specialist, bacteriologist. To begin with, it is recommended to contact a local pediatrician who will prescribe the necessary examination, and, if necessary, refer to other specialists. Diagnostics should be comprehensive - these are laboratory methods and instrumental diagnostics. Differential diagnostics are used, in particular, in most cases there is a need to differentiate streptoderma from other diseases of bacterial or fungal origin, as well as from various pyoderma, eczemas, from herpes.
The diagnosis is based on laboratory diagnostics, which consists of accurately identifying the qualitative and quantitative characteristics of the detected bacteria (bacteriological examination). The diagnosis of streptoderma is confirmed if streptococcus is isolated as the pathogen. As an additional research method, it is recommended to conduct an antibiotic sensitivity test. [ 1 ] It allows you to select the most effective antibacterial drug and its optimal dosage. It is usually carried out in combination with bacteriological culture.
Tests
Bacteriological culture is considered the main method of laboratory diagnostics of streptoderma, both in children and adults. The principle of the method is that skin scraping samples, or washes from the surface of the affected area, are inoculated on nutrient media, incubated, and then a pure culture is isolated with its subsequent identification. During the study, it is important to determine the exact species and genus of the microorganism, its quantity. [ 2 ] Along with bacteriological culture, it is advisable to conduct an analysis for antibiotic sensitivity (the drug that will be most effective for the isolated microorganism is selected, its optimal dosage is calculated). Based on this, further treatment is prescribed. This approach is considered the most rational, since it allows for the treatment to be as effective as possible. [ 3 ], [ 4 ]
Other research methods are also used. The gold standard of laboratory diagnostics is a clinical or general blood test, a biochemical blood test. Often these tests are used at the stage of early diagnostics, they allow to reveal the general picture of the pathology, the direction of the main pathological processes in the body. This analysis allows to effectively and most accurately prescribe additional research methods.
Sometimes a blood or smear test from the affected area is performed to check for sterility. [ 5 ], [ 6 ] The presence of bacteria is indicated by conventional signs:
- + means a small amount of bacteria,
- ++ means moderate amount of bacteria,
- +++ means high level of bacteria,
- ++++ is a sign of bacteremia and sepsis.
The presence of any of the indicated signs requires extended diagnostics and is the basis for prescribing a bacteriological study.
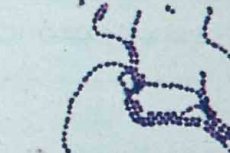
Microscopy of a smear from the affected area can have an important diagnostic value. This analysis allows the structure of the pathology. With the help of this analysis, not only bacteria are detected, but also cellular structures. It is also possible to identify hemolysis zones, indicating damage to blood vessels. It is possible to promptly identify the decay products of individual tissues, and promptly identify necrosis zones. Other methods are also used, but they are used mainly in dermatovenereological dispensaries, or other specialized departments and hospitals.
Anti-streptolysin O (ASO) antibody tests are of no value in the diagnosis and treatment of impetigo in children because the ASO reaction is weak in patients with streptococcal impetigo (Kaplan, Anthony, Chapman, Ayoub, & Wannamaker, 1970; Bisno, Nelson, Waytz, & Brunt, 1973) [ 7 ], presumably because streptolysin O activity is inhibited by skin lipids (Kaplan & Wannamaker, 1976) [ 8 ]. In contrast, anti-DNase B levels are elevated and thus may be evidence of recent streptococcal infection in patients suspected of having poststreptococcal glomerulonephritis.
Instrumental diagnostics
Instrumental diagnostics is an important additional method of research, without which it is impossible to make an accurate diagnosis. Instrumental diagnostic methods are used depending on the situation, if any concomitant pathology is suspected. Instrumental methods may include ultrasound of the kidneys, bladder, stomach, intestines, heart, rheography, electrocardiogram, Dopplerography, X-ray. Computer or magnetic resonance imaging, gastroscopy, colonoscopy, irrigoscopy, gastroduodenoscopy, endoscopy, and other methods may be required, especially if concomitant gastrointestinal diseases are suspected.
These methods are used to track changes in dynamics, obtain data on the structure and functional characteristics of the organs being examined. This makes it possible to judge the effectiveness of therapy, prescribe a particular treatment, and decide on the advisability of additional procedures and treatment of concomitant pathology.
Differential diagnostics
Using differential diagnostic methods, it is possible to differentiate the signs of one disease from the signs of another disease. Streptoderma must be differentiated, first of all, from herpes [ 9 ], atopic dermatitis [ 10 ] and from other types of bacterial diseases, from pyoderma of various origins, from fungal and protozoal infections. [ 11 ], [ 12 ]
The main method of differential diagnostics is bacteriological culture, during which the microorganism that caused the disease is isolated and identified. In case of a fungal infection, a fungus is isolated that is characterized by continuous growth and a white coating. Protozoan, parasitic infection is quite easily detected by conventional microscopy.
Streptococcal infection is characterized by a more severe course, a tendency to relapse. In most cases, streptoderma, unlike ordinary pyoderma, is chronic, with periodic exacerbations. Blisters with cloudy, green contents are formed. Numerous erosions and ulcers are formed, which, when healing, form crusts. Often, the infection also affects the mucous membranes: lips, corners of the mouth. Painful cracks and phlyctenas may appear. [ 13 ]
How to distinguish herpes from streptoderma in a child?
Many parents wonder how to distinguish herpes from streptoderma in a child? It is not surprising, because at first glance, the manifestations of these diseases are very similar. But it turns out that there are a number of differences in the clinical picture of the pathology. [ 14 ]
Herpes begins with severe itching, showing, often accompanied by severe pain. Then a red spot appears, similar to swelling. A large number of blisters appear on it, the size of a pin head. The blisters are filled with transparent serous contents. After 3-4 days, the blisters dry up, forming wet erosions. Also often the disease is accompanied by inflammation of regional lymph nodes, fever, chills, headache, malaise, muscle and joint pain (typical signs of a viral infection). The temperature can rise to 38-39 degrees. After 2-3 days, the crusts fall off, epithelialization occurs. The duration of the disease is usually 1-2 weeks. With streptoderma, the temperature rarely rises, often the child feels relatively well, malaise and weakness are not observed.
Herpes is most often located around natural openings - nose, lips, ears, eyes, often affects mucous membranes. Bacterial infection, in particular, streptoderma in children is usually localized throughout the body.

