
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Bacteria in the urine of a child: causes, how to treat
Medical expert of the article
Last reviewed: 12.07.2025
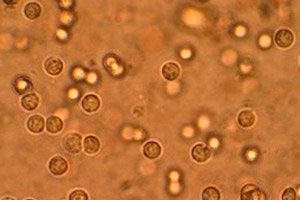
Clinical tests, including urine tests, help monitor the child's health. There are a number of external criteria by which certain deviations are determined: volume, color, odor, transparency, etc. Biochemical indicators are more informative, since they reveal protein, sugar, and bilirubin. The presence of bacteria in a child's urine is determined by microscopic examination of its sediment and is a dangerous signal. What does this mean? It indicates a viral disease of the urinary system. [ 1 ]
Normal levels of bacteria in a child's urine
The urine of a healthy child contains microorganisms. The bacterial count of urine properly collected in a sterile container should not exceed 100 units per milliliter of its volume. Exceeding this threshold is called bacteriuria and indicates the development of an infectious and inflammatory process in the urinary system. [ 2 ]
Epidemiology
According to statistics, about 20% of all hospitalized children are due to chronic cystitis. Up to 4% of the child population is susceptible to pyelonephritis. [ 3 ] In the structure of nephropathy, urinary tract infection ranks first. Among those who have bacteria in their urine, there are more girls than boys. [ 4 ]
Causes bacteria in the baby's urine
The most common reason for an increased number of bacteria in a child's urine is failure to observe hygiene rules when collecting it. A repeat analysis will either dispel suspicions or become a reason to look for another type of deviation, which may include:
- cystitis;
- urethritis;
- pyelonephritis;
- urolithiasis;
- inflammation of the external genitalia.
Risk factors
The factors that provoke the pathology include decreased immunity due to hypothermia, bacteria entering from the anus due to improper actions after defecation, ignoring hygiene procedures, bathing in dirty water. Sometimes the development of infection is caused by medical procedures performed without proper antiseptic measures, and even constipation due to improper nutrition. [ 5 ]
Pathogenesis
The infection can develop in an ascending way from the genitals or large intestine through the urinary tract upwards. Another way is descending, from top to bottom, for example, with kidney inflammation.
Symptoms bacteria in the baby's urine
As a rule, bacteriuria occurs with pronounced symptoms, but in some cases they may be absent. It manifests itself as frequent and painful urination, sometimes urinary incontinence, pain in the lower abdomen. The spread of infection to the kidneys leads to fever, nausea, vomiting, and pain in the lower back. [ 6 ]
Visually noticeable changes in the urine: it becomes cloudy, flakes float in it, there may be blood inclusions, and an unpleasant odor appears.
The presence of leukocytes, mucus, protein, and nitrites in the urine are sure signs of a urinary tract infection.
Complications and consequences
Detection of bacteria in urine requires immediate response, otherwise serious and dangerous health consequences are possible. Inflammation of the lower urinary tract without treatment can spread to the kidneys, and pyelonephritis is fraught with further complications, as a result of which you can even lose the organ.
Diagnostics bacteria in the baby's urine
The very first test for diagnosing a urinary tract infection (UTI) is a general urine test. It will reveal the presence of protein, an increase in leukocytes, and erythrocytes. Bacteria can be detected by microscopic examination of a culture medium. Its results are obtained only after 6-7 days, but they will indicate the causative agent of the infection, determine its sensitivity to antibiotics, which is necessary for the selection of drug treatment. [ 7 ]
There is also an express test for nitrites, but it is uninformative, since not all bacteria convert the nitrates contained in them into nitrites. You can't do without an ultrasound of the kidneys: their inflammation will show the expansion of the renal pelvis.
Differential diagnosis
The task of differential diagnostics is to determine which organ is affected by the inflammatory process and to make one of the above-mentioned diagnoses or others.
Who to contact?
Treatment bacteria in the baby's urine
Detection of bacteria in a child's urine and diagnosis requires a comprehensive approach to treating the infection, which includes not only drug therapy aimed at eliminating pain, normalizing urination disorders, eliminating the inflammatory process, but also organizing a healthy diet, drinking plenty of fluids, and using physiotherapy methods. [ 8 ]
Antibacterial therapy for pyelonephritis is longer than for cystitis or urethritis, and lasts 10-14 days versus a week of treatment. [ 9 ]
Drug treatment
The choice of antibiotic depends on the type of bacterial flora, but since it will only be detected a few days after the urine culture is taken, broad-spectrum drugs are initially prescribed, which are excreted primarily through the kidneys and are maximally concentrated in the bladder, and then, if necessary, the prescription is adjusted. [ 10 ]
Of the entire list of antibacterial drugs, the most commonly prescribed are amoxicillin, ciprofloxacin, cefaclor, ceftibuten, and monural. [ 11 ]
Amoxicillin - granules in a bottle for preparing a suspension are poured with purified water up to the mark on it and shaken until they are completely dissolved. Children under 2 years old are given half a measuring spoon (125 ml), from 2 to 5 years - a full one, 5-10 years - 1-2 spoons, older - 2 spoons three times a day.
For newborns and very young children, the dose is calculated as 30 mg of the substance per kilogram of body weight and is divided into 2 doses, with an interval of 12 hours between them.
Possible side effects include rashes on the body, nausea, bowel disorder, headache, tinnitus. Amoxicillin is contraindicated in case of hypersensitivity to its components, mononucleosis, lymphocytic leukemia.
Monural is a powder packaged in sachets. Before use, dissolve in half a glass of water. Recommended for the treatment of girls over 12 years old. Drink once a day on an empty stomach before bed after emptying the bladder. Side effects most often occur from the gastrointestinal tract in the form of diarrhea, dizziness is rare. Not prescribed for allergies to the drug.
Pain syndrome is relieved with antispasmodics: no-shpa, papaverine, belladonna, baralgin.
Baralgin - prescribed to children from 13 years old one tablet 2-3 times a day, after 15 years the dose can be increased to 2 pieces at a time, the frequency is the same. The drug can cause dry mouth, exacerbation of gastritis and peptic ulcer, tachycardia, visual impairment. An obstacle to the use of baralgin are blood diseases, severe kidney and liver pathologies, bronchial asthma.
To reduce inflammation, herbal preparations are also used. One of the popular ones is Urolesan.
Urolesan is a combined herbal preparation in the form of capsules, drops and syrup. For children, the most suitable form is syrup. It is taken before meals, the dose in the age range of 2-7 years is 2-4 ml, 7-14 years 4-5 ml three times a day. The drug is not used in case of allergy to the plants from which it is made (mint, fir, fruits of wild carrots, hops, oregano), gastritis with high acidity of the stomach, peptic ulcer, with caution in diabetes. [ 12 ]
Vitamins
Vitamins A (the daily dose should be at least 50 thousand IU), C (1-1.5 g) will help in the fight against pathogenic bacteria, but the main emphasis is on natural flavonoids - vegetables and fruits with bright colors (orange, purple, red).
Physiotherapy treatment
Hydrotherapy is widely used as a physiotherapeutic treatment, including the unique mineral water "Naftusya". Mineral baths, ozokerite and paraffin applications are also used. Electrophoresis and electrotherapy are effective.
Folk remedies
Many folk remedies are aimed at drinking plenty of fluids in order to flush the urinary tract of bacteria.
Here are some:
- squeeze the juice from the watermelon pulp and drink half a glass every 3 hours;
- mix 100 ml of carrot juice with a tablespoon of celery leaf juice, drink 3 times a day;
- Squeeze juice from 500g of fresh strawberries, drink half a glass 4 times a day.
Very effective is the treatment of UTI with herbs that have antimicrobial, anti-inflammatory, tanning, regenerating properties. These include bearberry, shepherd's purse, half-half, wild rosemary, chamomile, birch buds, lingonberry, juniper. They are used not only to prepare infusions and decoctions, but also to take warm sitz baths.
Homeopathy
Homeopathic remedies have proven themselves in the treatment of urinary tract infections. They not only help fight inflammation, but also increase the body's defenses and activate the processes of self-regulation of its functions. Among them are Berberis (barberry), Borax (borax), Cannabis sativa (hemp), Cantharis (Spanish fly), Equisetum (horsetail), Petroselinum (parsley), etc.
Only a homeopath can prescribe, since it depends not only on the symptoms and diagnosis, but also on the child's gender, anatomical features, and psycho-emotional state. In addition, most homeopathic remedies have not been tested on children, so they are recommended only for older children.
Surgical treatment
Only severe anomalies of the urinary tract require surgical correction; in other cases, conservative treatment is sufficient.
Prevention
In order to prevent urinary tract infection, you should drink plenty of fluids, avoid hypothermia, empty your bladder regularly, maintain hygiene of the external genitalia, and periodically use appropriate herbal remedies. Those who have had a UTI are recommended to undergo ultrasound examination of the kidneys and bladder for monitoring. [ 13 ]
Forecast
In most cases, the disease has a favorable outcome. The earlier the inflammation is detected and its active treatment is started, the higher the chance of not becoming chronic and not getting cicatricial changes in the kidneys with pyelonephritis.

