
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Babesiosis in humans - a dangerous but treatable disease
Medical expert of the article
Last reviewed: 04.07.2025
Among protozoan zoonotic diseases, babesiosis in humans is not as widely known as, for example, malaria or leishmaniasis.
Although parasitology encountered its pathogen in animals back in the late 19th century. And infectious disease doctors became convinced of the possibility of infecting people in the middle of the last century. And in the International Classification of Diseases (ICD-10), this acute transmissible disease was assigned the code B60.0.
Epidemiology
According to statistics provided by the International Society for Infectious Diseases, cases of babesiosis in humans are rarely recorded in Europe: since 1957, when the first case was accidentally detected (in what was then Yugoslavia), no more than four dozen cases have been officially registered, mainly in Ireland, Great Britain and France. It is noteworthy that all patients had a history of splenectomy.
Also, isolated cases with a pronounced clinical picture were registered in Mexico, Columbia, South Africa, Egypt, Korea, China and Japan. Most of the patients were over 45-50 years old.
In almost 20-25% of patients, babesiosis is combined with Lyme disease.
The global incidence of human babesiosis has increased over time. For example, there is no endemic human babesiosis in China, but over the past three decades, patients with the disease have been appearing with increasing frequency.
According to official data from the Center for Global Health (CDC), there were 5,542 cases of babesiosis in humans in the United States from 2011 through 2014.
Causes babesiosis
The only cause of babesiosis in humans is invasion, that is, the entry into the body of such a variety of protozoa as Babesia divergens and Babesia microti or babesia, belonging to the type Apicomplexa (or Sporozoea), genus Plasmodium, order Piroplasmidae.
The first subspecies is distributed on the European continent and in Asia, the second – in the Western Hemisphere, and both subspecies are found in Eastern and Northern Australia. Read more about this microscopic parasite (its hosts, biological cycle and reproduction) in a separate publication – Babesia.
The causative agent of babesiosis is carried by blood-sucking arthropods infected with protists, parasites of vertebrates - ixodid ticks: Ixodes ricinus (dog tick), Ixodes persulcatus (taiga tick), black tick (Ixode scapulari) and Ixodes pacificus, which prefers the Pacific coast.
It is clear that the routes of infection with babesiosis are transmissible - through tick bites in humans, when, together with the salivary fluid secreted during the bite, the Babesia sporozoites found in it enter the human blood.
Typically, the incubation period for the development of parasitemia after a tick bite is from one to four weeks, but sometimes it can be much longer.
In addition, other possible routes of infection include blood transfusions and organ transplants. Since 2003, the U.S. Centers for Disease Control and Prevention has documented over 40 cases of babesiosis following transfusions of stored plasma and two cases following allotransplants.
Risk factors
Infectious disease specialists consider living in or visiting endemic regions and weakened human immunity to be the main risk factors for contracting babesiosis. This includes not only HIV, but also chronic diseases of any internal organs and oncology that suppress the immune system, as well as immunosuppressive therapy.
It is almost impossible to resist this transmissible disease if a person has undergone a splenectomy, that is, his spleen (whose function is to destroy red blood cells that have served their time and died) has been removed.
As with other infections, children and the elderly are at increased risk of developing severe forms of babesiosis.
 [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ]
[ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ]
Pathogenesis
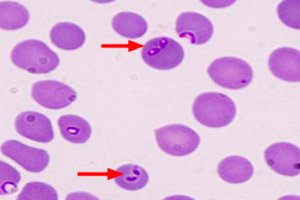
Explaining the pathogenesis of this disease, specialists note the ability of Babesia to penetrate not just into human blood, but into the cytoplasm of red blood cells. The number of affected blood cells is usually 3-10% of the total mass of red blood cells, but can vary from less than 1% to 85%.
Next, inside the red blood cells, the transformation of Babesia sporozoites into trophozoites and then into merozoites occurs. The growth of their numbers simply ruptures the red blood cells, and the reproductive cells of the parasite are carried by the bloodstream and attack new red blood cells.
The reproduction and pathological effects of babesia that enter the bloodstream cause an inflammatory reaction (due to the activation of proinflammatory cytokines) and hemolysis (massive death of red blood cells), which causes the clinical picture of babesiosis in humans.
Due to a sharp decrease in the level of red blood cells, hemolytic anemia is observed (leading to oxygen starvation of all tissues); the volume of bilirubin, a by-product of erythrocyte lysis, increases in the blood (which manifests itself as jaundice); toxic substances enter the blood, overloading the spleen and liver (with an increase in their size and a decrease in function). In addition, fragments of destroyed erythrocytes can accumulate in the capillaries and cause microvascular congestion.
With increased hemolysis, the kidneys can no longer cope with filtering the blood, which contains hemoglobin released from damaged red blood cells. This iron-containing and oxygen-carrying protein "clogs" the renal tubules, disrupting urine production and excretion.
Symptoms babesiosis
The severity of the disease and its manifestations depend on the state of the human immune system, and, according to some data, half of children and a quarter of previously healthy adults have no symptoms of babesiosis.
The first signs of this infection are non-specific and most often manifest as flu-like symptoms: general weakness and malaise; fever (constant or intermittent, with a temperature of up to + 40.5°C) – with chills and increased sweating; headache, muscle pain and joint aches; loss of appetite. Such a clinical picture can be observed from several days to several months.
Less common symptoms may include nausea, vomiting, abdominal pain; yellowing of the skin and darkening of the urine (if hemolytic anemia develops); the appearance of petechiae and ecchymosis; photophobia with reddening of the conjunctiva and hemorrhage in the retina; pain and redness in the throat or dry cough; stiffness of the occipital muscles; hyperesthesia; difficulty breathing; depression.
Complications and consequences
Severe cases can have multiple consequences and complications:
- congestive heart and respiratory failure, pulmonary edema and acute respiratory distress syndrome;
- acute renal, renal-hepatic or multiple organ failure;
- severe hemolytic anemia;
- thrombocytopenia or coagulopathy.
Spontaneous rupture of the spleen, myocardial infarction, and shock with fatal consequences may occur.
Patients with a removed spleen are in worse condition because the blood is not cleared of infected red blood cells. This leads to a higher degree of parasitemia, which ultimately causes hypoxemia and the subsequent threat of acute cardiopulmonary failure.
In addition, such patients may develop hemophagocytic syndrome, kidney failure and other organ failure, leading to coma.
In long-term babesiosis with organic damage to the brain, complications are neurological and mental in nature.
Diagnostics babesiosis
This infection is difficult to diagnose, and correct diagnosis of babesiosis requires high qualifications in the field of medical parasitology. Patient complaints and physical (palpation) examination of the spleen and liver are not enough to identify the true cause.
Blood tests are ordered in specialized laboratories that can adequately diagnose Babesia infection.
The following blood tests are required: complete blood count with differential (complete white blood cell count) and ESR; enzyme-linked immunosorbent assay (ELISA); PCR analysis; IgM ELISA, serological analysis for IgG and IgM; direct Coombs test; analysis for LDH (lactate dehydrogenase) level; for total bilirubin and haptoglobin; for serum creatinine and liver transaminases levels.
Urine tests are also performed to detect hemoglobinuria and proteinuria.
Confirmation of the diagnosis by a parasitologist is the detection of Babesia under a microscope in a peripheral blood smear.
Instrumental diagnostics – chest x-ray – may be required for patients with respiratory complications.
Differential diagnosis
Differential diagnostics are designed to exclude malaria, acute anemia, granulocytic anaplasmosis (ehrlichiosis), tick-borne borreliosis (Lyme disease), Q fever, and tularemia in the patient being examined.
Treatment babesiosis
Combined drug treatment of babesiosis is carried out taking into account the severity of the disease.
For mild and moderate forms, the following medications are used for 7-12 days: Azithromycin (a macrolide antibiotic) and Atovaquone (Atovaquone, Mepron, Malarone), an antiprotozoal hydroxynaphthoquinone agent.
Azithromycin is administered intravenously: 500 mg once a day (the first three days) and until the end of the course, 250 mg per day; the children's dose is calculated based on body weight. Atovacon is used at 750 mg every 12 hours.
For patients with severe babesiosis, parenteral administration of the lincosamide antibiotic Clindamycin (Cleocin) is necessary - 0.5-0.6 g every 8-12 hours; Quinine, Hingamin, Hinocid or Chloroquine phosphate (Chloroquine, Delagil) are taken orally - 0.5-1 g at the same intervals.
Antibacterial drugs are known to cause side effects: nausea, abdominal pain, intestinal disorders, etc. But their use in the form of injections somewhat smooths out the undesirable effects. Antiprotozoal drugs also have side effects, but without them, treatment of babesiosis is currently impossible. Although in case of severe allergy to quinine, a combination of Clindamycin + Doxycycline + Azithromycin is used.
The outcome of treatment is assessed by the results of blood smears for Babesia; if smears are negative for at least two weeks, then the therapy has been successful.
In case of high levels of parasitemia and hemolysis, to maintain the functions of the kidneys, liver and lungs in seriously ill patients, they resort to exchange blood transfusion.
Prevention
Prevention to reduce the risk of infection with Babesia involves the use of acaricidal repellents (with permethrin) to repel ticks - when people live, work or travel in areas where these arthropods are found, as well as during walks in wooded areas with grass cover (it is best to walk on paths).
Minimize the area of exposed skin: wear socks, closed shoes, long pants (tucked into socks) and a long-sleeved shirt. It is better to wear light-colored clothes, on which it is easier to notice a crawling tick. Treatment of the dog's fur and a special collar should protect the pet from ticks.
After going out of town or walking in the forest or park, you must shake out your clothes and carefully examine yourself and your pets.
Useful Information – What to Do After a Tick Bite
Forecast
Babesiosis has many serious consequences that affect the prognosis of the outcome of the disease.
Asymptomatic or subclinical infection in people with strong immunity can remain latent for a long time.
A mild form (without acute symptoms) can last for two or more months after treatment. A severe form of the disease does not exclude persistent relapses and can lead to death (5% of cases). But with a healthy spleen, such an outcome is rare, but the addition of non-specific pneumonia worsens the prospects for a quick recovery.
But babesiosis in a person with a removed spleen is more severe and often has concomitant infections: in such cases, the mortality rate can reach 50%.
Timely and correct diagnostics are extremely important. At the end of 2012, in Kyiv – after a tick bite and as a result of an initially incorrect diagnosis – a six-year-old child died from babesiosis.

