
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
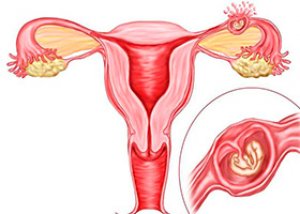
A tubal ectopic pregnancy
Medical expert of the article
Last reviewed: 04.07.2025
Symptoms tubal ectopic pregnancy
An ectopic pregnancy causes the same changes in a woman’s body as a uterine pregnancy: delayed menstruation, engorgement of the mammary glands, the appearance of colostrum, nausea, and taste perversion.
Progressive tubal pregnancy
During examination, cyanosis of the vaginal vestibule, vaginal mucosa and cervix is noted. The uterus increases in size, softens, the uterine mucosa is transformed into a decidual membrane. The corpus luteum of pregnancy is formed in the ovary, the immunological reaction to pregnancy is positive.
Interstitial tubal pregnancy
Interstitial tubal pregnancy before its interruption, which usually occurs in the 3rd-4th month, does not differ from a normal uterine pregnancy and therefore is not diagnosed. Its interruption occurs as an external rupture of the fetal sac, accompanied by profuse bleeding and has a clearly expressed clinical picture. An accurate diagnosis is usually established during surgery, when deformation of the uterus is detected due to protrusion of one of its corners, high separation of the ligamentous apparatus from the side of the lesion in the oblique position of the fundus of the uterus. The perforation hole can be of different sizes, but does not communicate with the uterine cavity; chorionic tissue often protrudes from the wound. Massive blood loss requires quick action from the gynecologist and anesthesiologist.
Rupture of the fallopian tube
A ruptured fallopian tube is characterized by an acute clinical picture of the disease. The patient suddenly experiences an acute attack of pain in the lower abdomen radiating to the rectum, cold sweat, pallor, and even a short-term loss of consciousness and a decrease in blood pressure (BP) are possible. The pulse becomes weak and frequent. BP may be reduced. Body temperature is normal or elevated. The phrenicus symptom is positive if there is at least 500 ml of blood in the abdominal cavity, symptoms of peritoneal irritation appear. In case of a disrupted tubal pregnancy, the patient's condition depends on the amount of blood loss: it can be satisfactory, moderate, or severe.
The abdomen is moderately distended, there is a mild tension of the muscles of the anterior abdominal wall and pain in the lower abdomen, more often on the side of the ruptured tube. In the lateral parts of the abdomen, dullness of percussion sound is determined (free blood in the abdominal cavity). The Shchetkin-Blumberg symptom is weakly expressed. During a gynecological examination (it should be carried out extremely carefully to avoid repeated pain shock, increased bleeding and collapse), a slight enlargement of the uterus is usually determined, its palpation and movements of the cervix are sharply painful. Through the lateral fornix of the vagina in the area of the appendages, pastosity and a tumor-like formation of a doughy consistency without clear contours are determined. The posterior fornix is flattened or even protrudes into the vagina. Palpation of the posterior fornix is sharply painful. Soon after the attack, minor dark bloody discharge appears from the cervical canal (they may be absent in the first hours). A few hours after the attack of pain, the decidual tissue, which is an almost complete cast of the uterine cavity, is rejected from the uterus. The patient's condition may stabilize or even improve for some time, but as internal bleeding increases, a picture of severe collapse and shock develops. The severity of the patient's condition is determined by the volume of blood loss, but the patient's ability to adapt to blood loss is of great importance.
An informative diagnostic test is culdocentesis, which confirms the presence of free blood in the abdominal cavity. The blood obtained by puncture is dark in color, contains soft clots and does not clot, which distinguishes it from blood obtained from a blood vessel (scarlet blood with rapid clot formation). If no blood is obtained as a result of puncture through the posterior fornix, this does not yet rule out the diagnosis of ectopic pregnancy, since the puncture may have been performed incorrectly or there may be no blood in the retrouterine cavity due to adhesions and growths in the pelvic area. Hemoperitoneum is considered an indication for emergency surgery. Rupture of the tube is a relative contraindication for organ-preserving surgery. Hemorrhagic shock of grades II–III is an indication for laparotomy. In this regard, the choice of surgical approach for rupture of the fallopian tube depends on the patient's condition.
Tubal abortion
Symptoms of tubal abortion consist of a combination of objective and subjective signs of pregnancy and symptoms of a terminated pregnancy. Usually, after a short delay in menstruation, cramping, periodically recurring attacks of pain in the lower abdomen appear, often unilateral. Scanty dark bloody discharge appears from the genital tract, caused by the rejection of the decidual membrane of the uterus. Tubal abortion, as a rule, lasts a long time, often without acute clinical manifestations. At the onset of the disease, blood from the detachment of the ovum from the fallopian tube enters the abdominal cavity in small portions, without causing sharp peritoneal symptoms and anemia of the patient. However, lability of the pulse and blood pressure, especially when changing body position, is considered a fairly characteristic sign. Further clinical manifestations of tubal abortion are determined by repeated bleeding into the abdominal cavity, the formation of a retrouterine hematoma and anemia. Symptoms of peritoneal irritation appear. During a vaginal examination, the size of the uterus is often enlarged. Sharp pain is noted when the uterus, its cervix and the posterior fornix are displaced. A sharply painful round formation is often palpated to the left or right of the uterus.
Diagnostics tubal ectopic pregnancy
Making a diagnosis of a progressive tubal pregnancy in the early stages is extremely difficult. In a progressive tubal pregnancy, the general condition is usually satisfactory. However, there are signs that are more characteristic of an ectopic pregnancy than of a uterine pregnancy:
- the hCG content is somewhat lower than during intrauterine pregnancy of the same duration;
- the increase in the size of the uterus does not correspond to the expected gestational age;
- In the area of the appendages, a tumor-like formation of a doughy consistency is palpated, painful upon examination.
Currently, due to the improvement of diagnostic quality (primarily ultrasound and hCG monitoring), it has become possible to diagnose a progressive tubal pregnancy. Reliable diagnostic signs are determined by ultrasound (determining the fertilized egg in the tube) and laparoscopy.
Dynamic monitoring of a patient with suspected progressive ectopic pregnancy is carried out only in a hospital with a 24-hour operating room, since its termination occurs suddenly and is accompanied by bleeding into the abdominal cavity.
When collecting anamnesis, the nature of the menstrual cycle, the number and outcome of previous pregnancies, the methods of contraception used are clarified, and the risk of ectopic pregnancy is assessed.
If the estimated pregnancy period is 3–4 weeks, there is no ultrasound data for intrauterine pregnancy and positive results of hCG in the blood, diagnostic and therapeutic laparoscopy is indicated.
The reaction to hCG in case of a negative result should be repeated several times. In modern conditions, the main treatment for progressive tubal pregnancy is considered to be organ-preserving surgery with endoscopic access.
Who to contact?
Treatment tubal ectopic pregnancy
The scope of the surgical intervention is excision of the uterine angle and application of two rows of separate catgut sutures to the wound: muscular-muscular and serous-muscular. Peritonization is performed with the involvement of the round ligament of the uterus.
More information of the treatment


 [
[