
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Bicornuate uterus and pregnancy
Medical expert of the article
Last reviewed: 04.07.2025
Bicornuate uterus and pregnancy is a pressing issue in obstetrics and gynecology, since this pathology causes a third of miscarriage cases in women with uterine malformations.
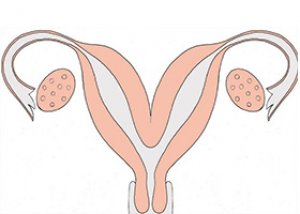
A bicornuate uterus is a congenital anomaly. The uterus begins to form from the Müllerian ducts of the embryo from about the 6th week of pregnancy. Due to genetic or teratogenic reasons, these ducts do not merge, which leads to bifurcation of the upper part of the uterus, and then the girl is born with uterus bicornuate - a two-horned uterus. And for adult women, a two-horned uterus, pregnancy and childbirth represent a chain of problems with the birth of children.
Bleeding with bicornuate uterus during pregnancy
The main cause of bleeding in a bicornuate uterus during pregnancy is considered to be placenta previa, which is a consequence of the implantation of the fertilized egg not in the area of the posterior and lateral walls of the body or fundus of the uterus, but in the endometrium of its lower part.
After implantation - from the 3rd week of pregnancy - the formation of the placenta begins, and the process of vascularization, that is, the formation of additional blood vessels, occurs inside the tissues of the uterine wall. If the embryo has settled too low in the uterus, the placenta (the formation of which is completed by the 13th week of pregnancy) can close its internal os. As a result, the pregnant woman experiences bloody discharge or bleeding (with pain in the lower abdomen). And this is the main harbinger of termination of pregnancy.
Bleeding with a bicornuate uterus during pregnancy most often occurs after 6-8 weeks of gestation and is observed in almost 35% of pregnant women. And partial placenta previa is observed on average in 40-45% of cases of pregnancy with a bicornuate uterus.
If bleeding with a bicornuate uterus during pregnancy occurs in the later stages (after 30-32 weeks), then its etiology is associated with the fact that the presenting part of the placenta cannot stretch as the size of the uterus increases and begins to peel off.
Bicornuate uterus and frozen pregnancy
A frozen pregnancy - that is, the cessation of fetal development and its death - in the presence of a complete or incomplete bicornuate uterus in a pregnant woman is a natural unfavorable outcome if the egg is attached not to the walls of the uterus, but to the septum.
The fact is that the tissues of these partitions do not have blood vessels, which means that the embryo cannot develop normally and dies.
In addition, a septum in a bicornuate uterus - when the embryo is located near it - can simply interfere with the natural process of fetal growth due to insufficient free space in the uterine cavity.
Bicornuate uterus and pregnancy
A bicornuate saddle-shaped uterus and pregnancy is the most favorable of the considered variants of this pathology. However, it can also lead to complications.
Obstetricians note that this type of bicornuate uterus can also lead to miscarriage (although much less frequently than with a complete or incomplete bicornuate uterus), and to fetal fading, and to premature birth. Thus, in 15-25% of pregnant women with a bicornuate saddle-shaped uterus, labor begins much earlier than expected. And this increases not only the overall perinatal morbidity of newborns, but also the risk of death of premature babies.
Also, this congenital pathology of the uterus affects the position of the fetus, and most often doctors state transverse or oblique presentation, in which case a cesarean section has to be performed. And after natural childbirth, such a uterus contracts very poorly and bleeds for a long time.
Bicornuate uterus and twin pregnancy
Twin pregnancy with the anatomical structure of the uterus, in the case under consideration – with a bicornuate uterus, does not have a direct cause-and-effect relationship. After all, the conception of twins is the result of fertilization of two follicles that matured simultaneously.
However, according to some data, twin pregnancy (mono- or fraternal) more often develops in women with anatomical pathologies of the uterine structure. In this case, the leading pathology is complete bifurcation of the uterus - that is, when the septum of the bicornuate uterus reaches the internal os or cervical canal with the formation of two separate cavities.
Bicornuate uterus and twin pregnancy are considered by obstetricians to be a group with a very high risk of miscarriage. Even uterine ruptures occur. And births after 32-34 weeks of twin pregnancy account for 90%.
As a result of many years of clinical observations, it has been established that the probability of fertilization of two eggs with a bicornuate uterus or its complete bifurcation is only one case in a million.
In cases where a bicornuate uterus and pregnancy - in terms of the ability to bear and give birth to a child - are mutually exclusive concepts, the woman may undergo an operation to restore the uterine cavity. This is an open (with an incision in the abdominal cavity) or hysteroscopic metroplasty. During this surgical intervention, the septum is dissected, and the uterus is "reconstructed" into a single cavity. In almost 63% of clinical cases, the reproductive capabilities of the uterus were completely restored.
Bicornuate uterus and pregnancy: features and complications
Among the pathologies that arise during intrauterine development, bicornuate uterus is quite common: it is detected in approximately 0.5% of women of childbearing age. Does this pathology affect the ability to conceive? Most experts claim that bicornuate uterus and pregnancy - in the sense of the ability to become pregnant - are not mutually exclusive concepts. Many women with such an anatomical defect of the reproductive organ both become pregnant and give birth. Here it is all about how deformed the uterine cavity is.
In a complete bicornuate uterus, there is a partition in its cavity (sometimes two-thirds of the cavity depth), which divides the uterus into two parts, and the fetus can develop in one of them. In an incomplete bicornuate uterus, a small division of the cavity is observed in its upper third. And the so-called saddle-shaped (or arcuate) bicornuate uterus has only a slight depression at the bottom of the cavity.
It should be noted that pregnancy with any of the three types of bicornuate uterus is associated with complications and requires additional medical monitoring. The risks include such unfavorable outcomes as habitual miscarriages (miscarriage rates reach 45-50% of cases) and frozen pregnancy (about 5%).
Bicornuate uterus and pregnancy have other complications. These are abnormal presentation of the fetus and premature birth. Breech presentation of the fetus is recorded in 50% of pregnancies with a partial bicornuate uterus. And in 40% there is a foot presentation, complicating the course of labor and threatening the newborn with asphyxia.
The number of premature births in the presence of a bicornuate uterus ranges from 25% to 35%. Doctors explain this by increased overstretching of the uterus, which has an irregular shape. Because of this, labor begins prematurely. Another factor that provokes premature birth is the inability of the isthmus and cervix to withstand internal pressure and hold the growing fetus until the due date (this is called isthmic-cervical insufficiency of the uterus). So, a cesarean section becomes the only way out in 65-70% of cases.
 [ 4 ]
[ 4 ]
Who to contact?

