
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Proteas
Medical expert of the article
Last reviewed: 06.07.2025
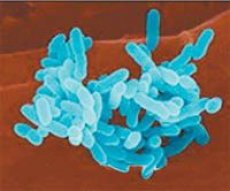
The genus Proteus belongs to the Enterobacteriaceae family and includes three species. Two species play an important role in human pathology, especially as causative agents of purulent-inflammatory diseases and food toxic infections: Proteus vulgaris and Proteus mirabilis.
All representatives of the genus Proteus are gram-negative rods with rounded ends, 0.4-0.6 x 1-3 µm in size, do not form spores or capsules, and are peritrichous. These bacteria are prone to polymorphism, and coccoid and filiform forms are observed. Sometimes non-motile variants, lacking flagella (O-form), are also encountered.
 [ 1 ]
[ 1 ]
Biochemical properties of protea
Facultative anaerobes, chemoorganotrophs. Temperature optimum 37 °C, pH 7.2-7.4; growth temperature limits from 20 to 38 °C. They are undemanding to nutrient media, grow well on simple media. The H-form (flagellate) Proteus produces a characteristic creeping growth on MPA in the form of a delicate veil of a bluish-smoky color (swarming phenomenon). The creeping growth of Proteus is used to isolate a pure culture when sowing according to the Shukevich method (the sowing is carried out in the condensation moisture of freshly mown MPA, the Proteus culture gradually rises in the form of a veil up the surface of the medium). The O-form of Proteus produces large colonies with smooth edges on MPA. On MPB, diffuse turbidity of the medium is noted with a thick white sediment at the bottom and a delicate film on the surface. The O-form of Proteus grows on certain nutrient media containing bile acids (Ploskirev's medium); 0.1-0.2% carbolic acid; 5-6% ethanol, dyes, boric acid, detergents. On Ploskirev's medium, Proteus produces transparent, delicate, shiny colonies with a characteristic odor, slightly alkalizing the medium, which is colored yellowish around them. With age, the colonies become cloudy, their center takes on a brown color. Colonies of Proteus in the O-form differ little from salmonella colonies, which complicates their identification. Kaufman, Muller, 5% bile broth are used as enrichment media.
Representatives of the genus Proteus ferment glucose to form acid and a small amount of gas, do not ferment lactose and mannitol, are resistant to cyanide, and form urease and phenylalanine deaminase. Species are differentiated by additional biochemical tests.
Antigenic structure of Proteus
Like other flagellated representatives of the Enterobacteriaceae family, Proteus has a heat-stable somatic O-antigen (49 serotypes) and a flagellar heat-labile H-antigen (19 serotypes). It should be noted that the somatic antigen of Proteus is related to the antigens of rickettsia (strains of Proteus of the OX series). According to their antigenic properties, Proteus vulgaris and Proteus ynirabilis are divided into 110 serotypes.
LPS of the Proteus cell wall is the most important pathogenicity factor, acting as an endotoxin.
Epidemiology of diseases caused by Proteus
Proteus are usually saprophytes of rotting waste, are present in small quantities in the intestines of animals and humans, and are found in wastewater and soil. Most often, infection occurs through the alimentary route, when a large amount of Proteus enters the human body with food. Proteus can often act as a causative agent of dysbacteriosis (endogenous infection) or as a typical causative agent of hospital infection.
Proteus is relatively stable in the external environment, tolerates freezing well. At a temperature of 60 °C it dies within 1 hour, at 80 °C - within 5 minutes, in a 1% phenol solution it dies within 30 minutes. It can be resistant to many antibiotics and disinfectants at the same time.
Symptoms of diseases caused by proteus
Proteus can cause various diseases in humans, most often occurring as food poisoning. In association with other opportunistic microorganisms, Proteus causes various forms of purulent-inflammatory and septic diseases: cystitis, pyelitis, purulent complications of wounds and burn surfaces, phlegmon, abscesses, pleurisy, pneumonia, osteomyelitis, meningitis, sepsis. The pathogenesis of food poisoning is associated with the massive destruction of Proteus in the gastrointestinal tract and the absorption of the endotoxin released in the blood. The severity of the disease is directly dependent on the amount of Proteus that has entered the body.
Laboratory diagnostics of diseases caused by Proteus
The bacteriological method is used. The material for sowing is pus, urine, vomit, washings, blood, cerebrospinal fluid, sputum, pleural exudate, which are inoculated on differential diagnostic media (Ploskirev medium), enrichment media and MPA according to the Shukevich method. The isolated pure culture is identified by biochemical properties, the serovar is determined in the agglutination reaction of a live and heated culture with polyvalent and monoreceptor O- and H-sera. It is also possible to determine the increase in O- and H-antibody titers in the agglutination reaction with autostrains.
Treatment of diseases caused by proteus
In case of food poisoning caused by Proteus, non-specific treatment aimed at detoxification is carried out (gastric lavage, drinking plenty of fluids, etc.). In case of a disease accompanied by suppuration or sepsis, antibiotics are used taking into account the results of the antibiogram. In case of colitis associated with intestinal dysbacteriosis, when Proteus is present in large quantities, it is advisable to orally use an intestinal bacteriophage, which includes the Proteus phage, as well as a Proteus or coliprotein bacteriophage. The latter drugs are also effective in local inflammatory processes (purulent complications of wounds, urogenital organs), when they are prescribed in the form of lotions, irrigations, tamponade, injections. In case of sluggish inflammatory processes that are difficult to treat with antibiotic therapy, it is advisable to use an autovaccine.

