
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Causes and pathogenesis of prostate adenoma
Medical expert of the article
Last reviewed: 04.07.2025
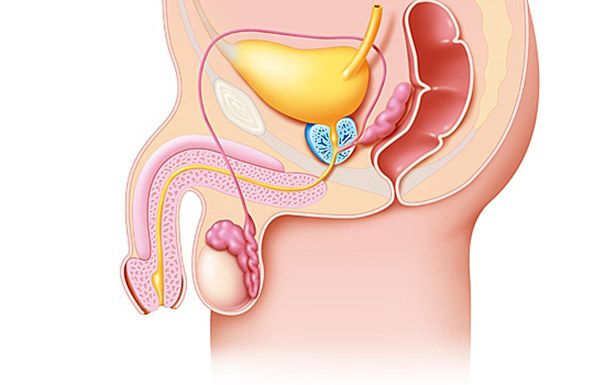
Understanding the pathogenesis of prostate adenoma (prostate gland) is impossible without taking into account modern data on its anatomy and morphology. The modern theory of prostate adenoma (prostate gland) development is based on the zonal concept of the prostate structure, according to which several areas are distinguished in the prostate gland, which differ in the histological and functional characteristics of the cellular elements that comprise them. These are the peripheral, central and transitional (transient) zones, as well as the area of the anterior fibromuscular stroma and the preprostatic segment.
In the area of the seminal tubercle, the outlet openings of the vas deferens open. The wall of the proximal part of the urethra consists of longitudinal smooth muscle fibers. The preprostatic (genital) sphincter, formed by a thick layer of smooth muscle fibers, surrounds the proximal part of the urethra from the neck of the bladder to the top of the seminal tubercle and prevents the occurrence of retrograde ejaculation.
Histological studies have shown that the growth of prostate adenoma (prostate gland) begins in the central and transitional zones of the prostate. The transitional zone of the prostate consists of two separate glands located immediately behind the internal sphincter of the bladder. The excretory ducts of this zone are located on the lateral wall of the urethra near the seminal tubercle. The proximal transitional zone contains the glands of the periurethral zone, they border the internal sphincter of the bladder and are located parallel to the axis of the urethra. Adenomatous nodes can develop both in the transitional zone and in the paraurethral zone. In addition to nodular hyperplasia, the transitional zone tends to grow with age.
The prostate capsule plays an important role in the development of prostate adenoma (prostate gland) symptoms. Thus, in dogs, the prostate capsule is poorly developed, and even with pronounced hyperplasia, symptoms of the disease rarely develop. The capsule transmits the pressure of the enlarged prostate tissue to the urethra, causing an increase in urethral resistance.
Prostate adenoma (prostate gland): pathophysiology
The prostatic part of the urethra is lengthened and deformed to 4-6 cm or more, mainly due to the area of the posterior wall located above the seminal tubercle. The neck of the bladder is raised and deformed, its lumen becomes slit-like. As a result, the natural curvature of the urethra increases, and with uneven development of the lateral lobes, the urethra also becomes curved in the transverse direction, as a result of which it can take on a zigzag appearance. Gaping of the lumen of the neck of the bladder as a result of the failure of the urethral-sphincter mechanism during detrusor compensation is clinically manifested by urinary incontinence.
The urinary bladder also undergoes profound changes. Its reaction to the development of obstruction goes through three stages: irritability, compensation and decompensation. At the first stage of infravesical obstruction, the urinary bladder responds by increasing detrusor contractions, allowing temporary maintenance of functional balance and complete evacuation of urine. Further development of obstruction leads to compensatory hypertrophy of the urinary bladder wall, which can reach 2-3 cm in thickness. In this case, it can acquire a trabecular appearance due to thickened and bulging muscle bundles.
The initial stage of trabecular development is morphologically characterized by hypertrophy of smooth muscle cells. Progression of the process leads to separation of hypertrophied muscle elements and filling of the spaces between them with connective tissue. Depressions called false diverticula are formed between the trabeculae, the walls of which gradually become thinner due to increased intravesical pressure. Such diverticula are often multiple, sometimes reaching significant sizes.
The elastic properties of the detrusor are determined by the presence of collagen, which in its smooth muscle tissue makes up 52% of the total amount of protein. As the compensatory capabilities are exhausted and atrophy increases, the walls of the bladder become thinner. The detrusor loses its ability to contract and stretches, as a result of which the capacity of the bladder increases significantly, reaching 1 liter or more. Concomitant inflammatory and trophic changes lead to pronounced sclerosis of the muscular layer of the bladder wall and a decrease in the collagen content. The content of connective tissue becomes equal to or exceeds the content of muscle elements.
The degree of restoration of the normal structure of the bladder wall depends on the duration of the obstruction to the urine outflow. As a result of prolonged obstruction, irreversible morphological changes develop, which lead to pronounced functional disorders of the bladder and cannot be eliminated even with surgical treatment. Severe infravesical obstruction leads to increased pressure in the bladder, impaired urine outflow from the kidneys and the development of vesicoureteral and renal reflux, as well as pyelonephritis. The ureters expand, lengthen, become tortuous, ureterohydronephrosis and chronic renal failure develop. The pathogenesis of changes in the kidneys and upper urinary tract in patients with prostate adenoma is complex and depends on many factors: age-related changes, concomitant diseases affecting their functional capacity, the development of obstructive uropathy.
At the first stage of obstructive uropathy, the preservation of the fornical apparatus of the calyces and the integrity of the epithelium of the collecting tubules of the papillae prevent the occurrence of renal pelvic refluxes and the penetration of infection into the renal parenchyma in an ascending manner. As ureterohydronephrosis develops, structural deformation of the calyceal vaults occurs, which creates favorable conditions for the occurrence of renal pelvic-tubular, and subsequently renal pelvic-venous and renal pelvic-lymphatic refluxes.
As a result of increased intrapelvic pressure and renal pelvis-renal reflux, renal hemodynamics are significantly impaired, followed by the development of structural changes in the intraorgan arteries in the form of their obliteration and diffuse stenosis. Hemodynamic disorders lead to serious metabolic shifts and severe renal tissue ischemia. Obstructive uropathy results in a progressive deterioration of all indicators of the functional state of the kidneys. A characteristic feature of this process is an early impairment of the renal concentrating ability, which is primarily manifested by a sharp decrease in the reabsorption of Na ions and an increase in their excretion with urine. Impaired renal function in stage I prostate adenoma is observed in 18% of patients. In stage II chronic renal failure complicates the course of the disease in 74%, with 11% of them having a terminal stage. Chronic renal failure is detected in all patients with stage III prostate adenoma, with the intermittent stage observed in 63% and the terminal stage in 25% of those examined.
Urinary tract infection is of fundamental importance in the pathogenesis of renal disorders in prostate adenoma and significantly complicates the course of the disease. Pyelonephritis and renal failure account for up to 40% of the causes of death in patients with prostate adenoma. Chronic pyelonephritis in patients with prostate adenoma is observed in 50-90% of cases.
Inflammation of bacterial origin occurs mainly in the interstitial peritubular tissue. In the pathogenesis of secondary pyelonephritis in prostate adenoma, the main role is played by urostasis, development of vesicoureteral and renal pelvis reflux. Infection enters the kidney ascending from the bladder. Urinary tract infection accompanies most cases of prostate adenoma. Chronic cystitis was observed in 57-61% of outpatients and 85-92% of inpatients. In this regard, the pathogenesis of chronic pyelonephritis in patients with prostate adenoma can be represented as follows: infravesical obstruction → bladder dysfunction → cystitis → insufficiency of the vesicoureteral junctions → vesicoureteral reflux → chronic pyelonephritis.
The presence of concomitant inflammatory process in the prostate plays a great role in the formation of the clinical picture in prostate adenoma. The frequency of chronic prostatitis in prostate adenoma according to laboratory, surgical and autopsy data is 73, 55.5 and 70%, respectively. Venous stasis, compression of the excretory ducts of the acini by hyperplastic tissue of the gland and its edema are prerequisites for the development of chronic inflammation. Morphological examination of the surgical material showed that in most cases the inflammatory process was localized on the periphery of the gland. Concomitant chronic prostatitis can clinically manifest itself as dysuria, which requires differential diagnosis with urination disorders caused by prostate adenoma itself. Its presence also leads to an increase in the number of early and late postoperative complications, in connection with which measures are needed to identify and sanitize chronic prostatitis at the stage of conservative treatment or preparation for surgery.
Bladder stones in adenoma are formed secondarily due to bladder emptying disorders. They are detected in 11.7-12.8% of patients. They usually have a regular round shape, can be single or multiple, and by chemical composition they are urates or phosphates. Kidney stones accompany prostate adenoma in 3.6-6.0% of cases.
A common complication of prostate adenoma is complete acute urinary retention, which can develop at any stage of the disease. In some cases, this is the culmination of the obstructive process in combination with decompensation of the contractile ability of the detrusor, while in others it develops suddenly against the background of moderate symptoms of urination disorders. Often, this is the first clinical manifestation of prostate adenoma. According to the literature, this complication is observed in 10-50% of patients, most often it occurs at stage II of the disease. Provoking factors for the development of this complication can be a violation of the diet (intake of alcohol, spices), hypothermia, constipation, untimely emptying of the bladder, stress, taking certain medications (anticholinergic drugs, tranquilizers, antidepressants, diuretics).
The main factors in the development of acute urinary retention are the growth of hyperplastic tissue, functional changes in the tone of the neck and muscle of the bladder, and impaired microcirculation of the pelvic organs with the development of prostate edema.
In the initial stage of acute urinary retention, increased contractile activity of the detrusor leads to an increase in intravesical pressure. In subsequent stages, due to stretching of the bladder wall and a decrease in its contractile ability, intravesical pressure drops.

