
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
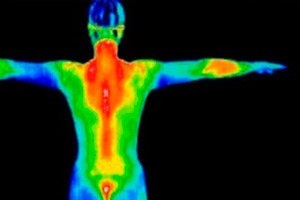
Thermal imaging (thermography)
Medical expert of the article
Last reviewed: 07.07.2025
In 1960, military engineer R. Lawson was testing a night vision device that was secret at the time and accidentally pointed the receiving lens of the device at a lady with an open décolleté sitting opposite him. A thermogram of the mammary gland appeared on the device’s screen. This phenomenon interested the major. Having understood the prospects of this direction, he left the service and already in 1961, together with R. Barnes, he developed and successfully applied in practice the first installation for medical thermography.
Indications for the procedure
The most commonly used areas of diagnostic use of thermal imaging are the following.
- Recognition of precancerous and tumorous lesions of the mammary glands, thyroid glands, orbit and some skin diseases.
- Diagnosis of joint diseases.
- Detection of initial and/or advanced stages of stenotic/occlusive lesions of the carotid, subclavian, femoral and popliteal arteries.
- Diagnosis of venous discirculation in the limbs and scrotum.
As can be seen from the above list, the "neurological aspect" of the studies is represented only by the detection of carotid insufficiency. Without in any way diminishing the importance of detecting stenotic/occlusive lesions of the carotid arteries, which are known to often proceed asymptomatically or with few symptoms, we believe we have the right to significantly expand the range of thermographic studies in neurology.
It is known that the classics of neurology considered it mandatory to examine the patient naked, so as not to miss any hypotrophy, dysraphism, etc.
Just as the basis of a neurological examination is the determination of various asymmetries in the cranial nerves, motor and/or sensory spheres, the identification of anisotherms in various areas of the patient’s body is the essence of thermography.
If we take into account that thermography is an extremely sensitive method (measurement accuracy up to 0.01 °C) with a relatively lower specificity, the analysis of thermograms becomes a creative process that requires an essential clinical analysis of the situation in each specific case.
For example, orbital anisothermia can be caused by completely different processes - from carotid artery occlusion to a tumor of the superior orbital fissure, from lagophthalmos to cluster migraine. Given the simplicity, short duration, safety, painlessness and availability of thermal imaging, diagnosticians consider this method ideal for mass random examinations of the population to detect early stages of oncological, vascular, inflammatory diseases of the chest, thyroid glands, kidneys, joints, scrotum, limbs.
In this case, highly sensitive corporal thermography would become indispensable for the rapid preliminary selection of patients: in the case of anisothermia of the head, these are the most likely patients of a neurologist, neurosurgeon, ophthalmologist or otolaryngologist; in the case of temperature asymmetry of the neck or mammary glands, patients are referred to an endocrinologist or oncologist; and those with anisothermia of the extremities are likely patients of angiologists.
Methodology of implementation
Thermography is the registration of invisible infrared radiation. The maximum radiation is at a wavelength of 9.5 microns. According to the Stefan-Boltzmann law, the amount of emitted energy is proportional to the fourth power of the absolute temperature: W=T 4.
Infrared radiation of the skin does not depend on race, degree of pigmentation and other individual characteristics. The temperature of the body surface depends on 3 main factors: vascularization features, level of metabolic processes and differences in thermal conductivity.
Currently, 3 modifications of recording infrared radiation of the body are used.
- Thermography records thermogenesis of the most superficial layers of the skin (0.5-1.5 mm).
- Infrared radiometry in the centimeter and decimeter range (wavelength 17 cm with a frequency band of 1.5-2.0 kHz) allows obtaining information about the deep structures of the body.
- Film thermography using contact liquid crystal strips records thermal radiation from the outer layers of the skin with a thickness of 0.3-0.8 mm.
There are basic types of thermal imaging devices.
- Thermographs that use liquid nitrogen to cool the temperature-sensitive sensor. These devices allow you to get a distant picture of the infrared glow of the examined part of the human body. They are good for examining planned patients in a hospital and/or outpatient clinic, but are of little use in emergency medicine, especially at the patient's bedside. A significant limitation is the need for constant availability of a fairly scarce, easily evaporated liquid nitrogen.
- Thermographs that do not require the use of liquid nitrogen. Such devices provide contactless display of the infrared activity map of the spectrum being studied. Portable thermographs are especially convenient - universal devices for emergency medicine: examination at home, in an ambulance, admission department, hospital, clinic, intensive care, operating room. The specified devices are portable, highly sensitive, and fairly easy to maintain. The sensitivity of these systems is quite high and reaches hundredths of a degree.
- Contact thermography based on liquid crystal films. There are domestic and foreign analogues. Advantages - lower cost of research, no need to use liquid nitrogen. Disadvantages - labor intensity, the possibility of using only on a flat surface, the need for tight uniform contact with a dry skin surface, difficulty of use in emergency medicine. This modification of thermal imaging has lower sensitivity - about 0.5 °C.
- Infrared radiometry, or thermotomography. This type of thermograph has a special antenna that records ultra-high frequency ranges, which allows measuring the temperature of body structures up to 17 cm deep with an accuracy of 0.1 °C. Unfortunately, this device is very sensitive to interference, so the results become reliable only when working in a special shielded chamber.
Evaluation of results
Normally, the distribution of temperature activity of identical areas of the human body is strictly uniform. Therefore, the essence of medical thermography basically comes down to identifying, localizing and determining the degree of thermal asymmetries and their clinical assessment. In healthy people, features of symmetrical heat distribution are noted. Thus, the orbital region, facial skin, lips, neck are usually warmer (appear as light areas) than the nose, upper forehead, outer segments of the face (dark areas).
In parallel, the most typical and constant temperature gradients of the thermograms of the head and extremities are taken into account.
- Horizontal orbital gradient. Normally, with uniform infrared glow of the orbits, the temperature of the inner corner of the eye is 0.3-0.7° higher than the outer one.
- Longitudinal gradient of the upper extremities. The shoulder is usually 0.5-0.7° "hotter" than the back of the hand.
- Longitudinal thermal gradient of the lower extremities. In most healthy people, the thigh temperature is 0.6-1.1° higher than the foot temperature.
The above gradients are relative. If the orbital one is the most constant, then the "limb" anisothermia is variable. This is especially true for the hands - the main "heat exchanger" of the body. Thermogenesis of the hands is most susceptible to fluctuations due to innervation, psychoemotional, medicinal and cold effects.
A number of pathological conditions that cause changes in the infrared activity of various parts of the patient's body.
Occlusion of the internal carotid artery or stenosis of more than 70% is usually accompanied by hypothermia of the orbit on the side of occlusion with a thermal gradient of 1.5-2.7°. During carotid endarterectomy, there is a direct relationship between the "luminosity" of the orbit and the superciliary region (vascularization zones of the angular and supratrochlear arteries) and the degree of narrowing of the lumen of the carotid artery. With a narrowing of the lumen of the internal carotid artery of more than 60%, a decrease in infrared radiation of the orbital region homolateral to the stenosis is noted.
E. Wood, using a combination of thermography and angiography, showed that in cases where the homolateral external carotid artery serves as a collateral for the occluded internal carotid artery, its short-term compression further increases the “cooling” of the orbit on the side of the affected artery.
When examined during an exacerbation, cluster headaches show a pronounced increase in luminescence of up to 1.5-2.0° on the side of the “pain clusters”.
On the contrary, a rare but extremely interesting pathogenetically cold migraine (ace cream headache), arising as a result of proven spasm of the siphon of the internal carotid artery, gives a pronounced transient hypothermia of the orbit on the side of pain.
Temporal arteritis is usually accompanied by the detection of “severe” hyperthermia in the projection of the superficial temporal artery.
Persistent, severe hypothermia of the Harlequin mask type is characteristic of Barraquer-Simons syndrome.
Characteristic changes in the thermogram of the head are observed in venous cerebral discirculation - pulsating exophthalmos, Tolosa-Hunt syndrome and Melkersson-Rosenthal syndrome. In the latter case, hyperemia of the lips and tongue during exacerbation of the edematous syndrome gives a clear hyperthermia, which is leveled by pathogenetic therapy.
The most common forms of facial damage are prosopoparesis and trigeminal neuralgia. They have vague thermographic signs - from pronounced local hyperthermia in the superciliary region during exacerbation of neuralgia of the first branch of the trigeminal nerve to relative hypothermia on the side of pain of its second and third branches. Prosopoparesis for the most part does not lead to significant facial anisothermia.
In patients with an exacerbation of vertebral artery syndrome, areas of hyperthermia are most often noted in the paravertebral zone C4 - C5 on the side of the pain syndrome.
When studying thermograms of the extremities in patients with acute cerebrovascular accident, we first noticed pronounced early hypothermia in the left extremities of patients with right-sided hemispheric hemorrhages. On the one hand, this phenomenon allows us to assume the probable localization of the hematoma in the case of deep coma, on the other hand, it confirms the well-known thesis about the functional asymmetry of the hemispheres with the predominance of the centers of vegetative regulation in the right hemisphere.
In some observations of patients with the posterior corneal form of syringomyelia, we were the first to register anisothermia of the torso in the form of a half-jacket, confirming segmental-dissociated sensitivity disorder in this disease.
The most striking changes in thermograms were noted in metastatic lesions.
Raynaud's syndrome produces pronounced asymmetric changes in the thermograms of the hands, especially after a cooling test, when instead of quickly warming up the hands after a 10-minute immersion in cold water, the fingers do not warm up as normal (due to the rapid opening of arteriovenous shunts), but remain hypothermic for a long time.
For most patients with vibration disease, in contrast to Raynaud's syndrome, symmetrical hypothermia of the hands is more characteristic, up to "thermal amputation" during an exacerbation.
As already mentioned, thermogenesis of the hands is dynamic. In this regard, the most important aspect of hand thermal imaging is the possibility of using dynamic thermography and ultrasound in anti-nicotine propaganda.
Hot feet are typical for patients with erythromelalgia. Thermography is very informative in dynamic observation of patients with angiopathies of the distal parts of the lower extremities of various genesis, it demonstrates the effectiveness or failure of drug and/or medicinal treatment.
The following two aspects of thermal imaging application are important not only for urgent neurology, but also for emergency medicine in general. Firstly, we are talking about the possibility of non-invasive diagnostics of subclinical stages of iatrogenic thrombophlebitis. Dynamic thermal imaging and ultrasound duplex monitoring of a catheterized vein showed that post-injection phlebitis occurs in 50% of patients on the 2nd day of continuous catheterization. Hyperthermia areas along the catheterized vein, recorded on the thermogram, together with impaired venous outflow according to ultrasound duplex examination, reflect the development of iatrogenic phlebitis. Timely treatment helps prevent further development of phlebothrombosis, and repeated thermal imaging control helps assess the effectiveness of preventive treatment.
Dynamic thermal imaging and ultrasound monitoring of venous circulation in the lower extremities of patients with hemiplegia is no less important. Studies supplemented by ultrasound Dopplerography, duplex examination and coagulation tests have shown that 60% of patients with hemiplegia develop a prethrombotic state already on the 2nd-3rd day of stroke, and 6 times more often in the paralyzed lower extremity. This is understandable, because in neurological patients, clinical recognition of phlebopathy is difficult due to sensory and motor disorders. Moreover, this is often combined with speech impairment. As a result, unlike patients in therapeutic and surgical departments, neurological patients, as a rule, do not present alarming complaints of swelling, pain and similar sensations. Therefore, if dynamic thermography and ultrasound methods reveal even the initial signs of venous outflow disturbance, urgent preventive treatment is necessary to prevent the development of such a formidable complication of emergency medicine as pulmonary embolism.
Research in recent years has convincingly shown that if the death of a person as an individual, but not as an organism, is inextricably linked with the death of the brain, then cerebral death is completely associated with the cessation of intracerebral blood flow and the registration of the so-called stop phenomenon, which until now has been established only with the help of contrast cerebral angiography. Obviously, such an unsafe and difficult to implement procedure is unacceptable for seriously ill patients.
Non-invasive ultrasound methods and thermography are obviously more ethical, accessible and informative.


 [
[