
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The retina of the eye
Medical expert of the article
Last reviewed: 06.07.2025
The retina (retina, retinal membrane) is a peripheral part of the visual analyzer. It develops from the anterior part of the cerebral vesicle, so it can be considered a part of the brain that is located on the periphery.
The inner (sensitive) membrane of the eyeball (tunica interna, s. sensoria bulbi), or retina, is tightly adjacent to the choroid on the inner side along its entire length - from the exit of the optic nerve to the edge of the pupil. In the retina, developing from the wall of the anterior cerebral vesicle, two layers (sheets) are distinguished: the outer pigment part (pars pigmentosa), and the complexly structured inner light-sensitive part, called the nervous part (pars nervosa). Accordingly, the functions distinguish the larger posterior visual part of the retina (pars optica retinae), containing sensitive elements - rod-shaped and cone-shaped visual cells (rods and cones), and the smaller - "blind" part of the retina, devoid of rods and cones. The "blind" part of the retina (pars ciliaris retinae) unites the ciliary part of the retina (pars ciliaris retinae) and the iris part of the retina (pars iridica retinae). The boundary between the visual and "blind" parts is the serrated edge (oga serrata), which is clearly visible on the preparation of the opened eyeball. It corresponds to the place where the choroid proper transitions into the ciliary circle of the choroid.
The retina is divided into an outer pigment part and an inner light-sensitive nerve part.
The first layer of pigment epithelium is adjacent to Bruch's membrane - the choroid. Pigment cells surround photoreceptors. Pigment layer cells phagocytize the rejected outer segments of photoreceptors, transport metabolites, salts, oxygen, and nutrients from the vascular membrane to the photoreceptors and back.
Bruch's membrane separates the retinal pigment epithelium from the choriocapillaris and, according to electron microscopy, consists of 5 elements:
- Basal lamina of the retinal pigment epithelium.
- Inner collagen layer.
- Thick layer of elastic fibers.
- Outer collagen layer.
- Basal lamina of the outer layer of the choriocapillaris.
The retinal pigment epithelium is a single layer of hexagonal cells whose villous apparatus surrounds the outer segments of the photoreceptors, ensuring their renewal. The density of retinal pigment epithelium cells in the fovea is lower, they are larger and contain more large melanosomes than retinal pigment epithelium cells in other parts of the retina. The connection between the retinal pigment epithelium and the photoreceptors is less dense than between the retinal pigment epithelium and the underlying Bruch's membrane. The conditional space between the retinal pigment epithelium and the sensory retina is called the subretinal space. The absence of fluid in the subretinal space is maintained in two ways:
- The cells of the retinal pigment epithelium and the intermediate dense junctional complex (zonula occludentes) form the external hematoretinal barrier, which prevents the release of extracellular fluid from the chorioretinal vessels into the subretial space.
- Active transport of ions and water from the subretinal space.
The second layer is formed by the outer segments of photoreceptors, rods and cones. Rods have very high light sensitivity, so they provide twilight vision. In addition, rods make up the bulk of neuroepithelial cells and are located throughout the retina to the borders of its optical part, providing peripheral vision. Cones perform a more subtle function of the eye: central, shaped vision and color perception. Cones are located mainly in the area of the central fovea of the macula.
Third layer. Towards the periphery, the number of cones decreases, and the number of rods increases. In the central fovea itself, there are only cones, then cones are found among the rods, and in the peripheral zone of the retina, cones are absent. That is why the central fovea has the best acuity of visual acuity, and the field of vision for colors is significantly narrower than for white.
The third layer, the external limiting membrane, is a band of intercellular adhesions. It is called Verhoer's fenestrated membrane because the outer segments of the rods and cones pass through it into the subretinal space (the space between the rod and cone layer and the retinal pigment epithelium), where they are surrounded by a substance rich in mucopolysaccharides.
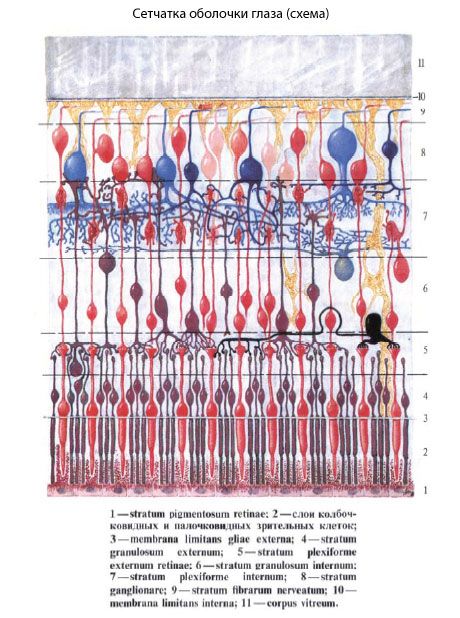
The fourth layer - the outer nuclear - is formed by the nuclei of the photoreceptors.
The fifth layer, the outer plexiform (or reticular) layer, occupies an intermediate position between the outer and inner nuclear layers.
The sixth layer consists of bipolar cells, each of which has two processes. The cells of this layer connect two neurons: the first with the third. The number of bipolar cells is less than the number of rods, so one bipolar cell is connected by several cells of the rod elements, while each cone has its own bipolar bead. The nuclei of the bipolar cells make up the middle nuclear layer of the retina.
The seventh layer, the inner plexiform layer, separates the inner nuclear layer from the ganglion cell layer and consists of a tangle of complexly branching and intertwined neuronal processes. It separates the inner vascular part of the retina from the outer avascular part, which depends on the choroidal circulation of oxygen and nutrients.
The eighth layer is formed by ganglion cells. They are located in a single row with gaps, with the exception of the area immediately around the central fovea, where the ganglion cell layer lies in 3-4 rows, so in this area it is thicker than the others. The nuclei of the ganglion cells make up the inner nuclear layer of the retina; the ganglion cells of the retina, like other cells of the retina, have a typical structure. These are round cells, rich in protoplasm, with a round nucleus and a well-developed chromatin structure. The thickness of the ganglion cell layer decreases noticeably as it moves away from the central fovea to the periphery. Around the fovea, this layer consists of five or more rows of ganglion cells. In this area, each photoreceptor has a direct connection with a bipolar and ganglion cell.
The ninth layer consists of the axons of the ganglion cells that form the nerve.
The tenth layer - the internal limiting membrane - covers the surface of the retina from the inside. It is the main membrane formed by the bases of the processes of the neuroglial Müller cells. These cells pass through all layers of the retina, are gigantic in size and perform supporting and isolating functions, carry out active transport of metabolites at different levels of the retina, and participate in the generation of bioelectric currents. These cells completely fill the gaps between the neurons of the retina and serve to separate their receptive surfaces.
Landmarks
- The macula is a rounded area at the posterior pole of the eye, approximately 5.5 mm in diameter. Histologically, it contains more than one layer of ganglion cells and xanthophyllic pigment.
- Fovea is a depression on the inner surface of the retina in the center of the macula with a diameter of 1.5 mm (1 diameter of the optic nerve disk). Ophthalmoscopically it looks like an oval light reflex, the boundaries of which are determined by the thickening of the retina and the internal limiting membrane.
- The foveola, 0.35 mm in diameter, forms the central part of the fovea. It is the thinnest part of the retina, devoid of ganglion cells and consisting only of cones.
- The foveal avascular zone is located within the fovea, extending beyond the foveola. The diameter of the foveal avascular zone is variable and can only be accurately determined using fluorescein angiography.
- The pit is a small depression in the very center of the foveola, corresponding to the foveolar reflex. The absence of the reflex can sometimes be interpreted as an early symptom of the disease.
The internuclear layers of the retina consist of fibrous structures, processes and synaptic formations of nerve cells, as well as cells of the glial skeleton of the retina, the fibers of which run perpendicular to the layers through the entire thickness of the retina: from the outer limiting membrane, separating the nuclei of the neuroepithelium from the rod and cone endings, to the inner one, separating the retina from the vitreous body.
The total number of rods is about 130 million. They are the receptors of twilight vision. Rods are characterized by the presence of a relatively small nucleus surrounded by a rim of cytoplasm. The dendrites of the rods have a radial orientation and are located between the processes of the retinal pigment epithelium. The dendrite consists of outer and inner segments (parts) connected by a cilium. The outer segment has a cylindrical shape. It consists of numerous double membranes superimposed on each other to form closed disks. The membranes of the outer segments contain rhodopsin, a visual pigment. The axon of the rods ends in the outer retinal layer of the retina with synapses with bipolar cells.
The number of cones in the retina is 6-7 million. They are the receptors of daytime (color) vision. Unlike rods, cones are larger (up to 75 µm in length) and have a larger nucleus. The outer segment of the cones is represented by semi-disks formed as a result of invagination of the plasma membrane. The membranes of the cone disks contain another visual pigment - iodopsin. In the inner segment, the cones have a cluster of mitochondria with a lipid droplet (ellipsoid) located here. The axon of the cones also forms synapses with the dendrites of bipolar neurons.
In the posterior part of the retina at the bottom of the eyeball in a living person, using an ophthalmoscope, you can see a whitish spot about 1.7 mm in diameter - the optic nerve disc (discus nervi optici) with raised, ridge-shaped edges and a small depression (excavatio disci) in the center. The disc is the place where the optic nerve fibers exit the eyeball. The optic nerve is surrounded by membranes (a continuation of the membranes of the brain) and is directed towards the optic canal, which opens into the cranial cavity. These membranes form the external and internal sheaths of the optic nerve (vagina externa et vagina inlerna n. optici). The area of the optic nerve disc, due to the absence of light-sensitive visual cells (rods and cones), is called the blind spot. In the center of the disc, the central artery (a. centralis retinae) entering the retina is visible. Lateral to the optic disc by approximately 4 mm, which corresponds to the posterior pole of the eye, there is a yellowish spot (macula) with a small depression - the central pit (fovea centralis). The central pit is the place of the best vision: only cones are concentrated here, and rods are absent.
The functions of the retina are the transformation of light stimulation into neural excitation and primary processing of the signal.
What's bothering you?
What do need to examine?


 [
[