
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Pericardectomy
Medical expert of the article
Last reviewed: 06.07.2025
Cardiovascular diseases occupy one of the first places in the general structure of pathologies. Therefore, cardiology is considered the leading direction in medicine in any country in the world. There are many known cardiac diseases that affect people of almost all ages, and one such pathology is pericarditis, which affects the pericardium, or the outer shell of the heart. In chronic pericarditis or purulent form of the disease, one of the treatment methods can be pericardiectomy - surgical correction, a fairly complex operation performed by a cardiovascular surgeon. [ 1 ]
The pericardium is a pouch-like structure that contains the heart. The purpose of such a sac is to protect and ensure normal cardiac function. Disturbances in this area negatively affect the organ's blood supply and can cause the development of purulent complications and the formation of fibrotic adhesions. To prevent the development of life-threatening conditions, pericardiectomy is prescribed - a surgical intervention during which the pericardium is removed - partially or completely. [ 2 ]
Indications for the procedure
The affected parts of the pericardium are removed only in extreme cases, when there is danger and threat to the patient's life. According to indications, the entire sac can be removed - such an operation is called subtotal pericardiectomy. When only the affected parts are excised, the Rena-Delorme operation is performed. By the way, the first type of operation, which involves complete removal of the pericardium, is practiced more often, as it allows preventing further obstructive changes. Both types of intervention are quite complex, the patient is carefully prepared for them, and after the operation, long-term observation is established.
The basic indications for performing pericardiectomy are exudative and constrictive forms of pericarditis. We are talking about pathological conditions accompanied by the accumulation of exudate, blood or fluid in the pericardial space. This leads to disruption of cardiac blood supply, formation of adhesions, and an increased risk of patient death as a result of myocardial infarction or heart failure. The signs of pericarditis are as follows: changes in blood pressure in one direction or another, severe shortness of breath, arrhythmia, pain and heaviness behind the sternum.
In turn, the causes of pericarditis may be viral or other infections, chest injuries, metabolic disorders, renal failure, connective tissue diseases, Crohn's disease, etc. [ 3 ]
Preparation
Since pericardiectomy surgery is very complicated and involves a lot of risks, the patient is given a number of diagnostic tests beforehand. It should be noted that pericardiectomy should always be clearly indicated, and the doctor must make sure that the patient has no contraindications.
If there is an accumulation of exudative fluid in the pericardial area, the surgeon may first perform a puncture. This is necessary to clarify the origin of the fluid and to remove it. Some time before the pericardiectomy, the patient is prescribed diuretics and medications to improve cardiovascular function.
When admitted to the surgical department, the patient is offered a series of tests. Typically, these tests include chest X-ray, electrocardiography, echocardiography (if necessary, an esophageal probe is used), and certain clinical and biochemical laboratory tests.
All women over 45 and men over 40 undergo cardiac catheterization, coronary angiography, and in some cases, aortography and ventriculography. If the diagnosis reveals damage to the coronary arteries (narrowing or blockage), the surgeon will adjust the surgical treatment plan and perform additional aortocoronary bypass surgery with the creation of bypass circulatory pathways.
The patient is prohibited from drinking alcohol for a week before pericardiectomy. It is strongly recommended to stop smoking or at least minimize the number of cigarettes smoked.
An important stage of preparation for pericardiectomy is nutrition. Doctors advise not to overload the digestive tract before the operation, avoid overeating and eating heavy (fatty, meaty) food.
The day before the procedure, the patient should not eat or drink anything. In the morning, he takes a shower and shaves the hair in the chest area (if required). [ 4 ]
Technique pericardectomies
Pericardiolysis, or Rena-Delorme, is a variant of partial pericardiectomy that involves partial excision of the pericardium, with separation of the cardiac-pericardial adhesions. In this situation, pericardial removal is performed only in certain areas.
In subtotal pericardiectomy, almost the entire pericardium is excised. This type of intervention is the most common: after the operation, only a small portion of the pericardium remains, localized at the posterior cardiac surface.
Pericardiectomy is performed using general anesthesia, and the patient is prepared for this in advance. On the day of the operation, the patient takes a shower, changes into sterile underwear and goes to the preoperative ward, where all necessary procedures are performed.
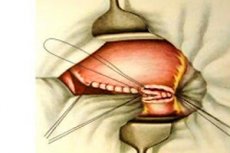
The patient is put under endotracheal anesthesia, connected to a ventilator, and a device is attached to monitor heart rate and blood pressure. The surgeon then proceeds directly to the pericardiectomy operation by access through the sternum or through the two pleural route with a transverse sternal intersection:
- a small incision (up to 2 cm) is made above the left ventricle, which allows the epicardium to be opened;
- the surgeon finds the layer separating the pericardium from the epicardium, then grasps the pericardial edges with an instrument and moves them apart, separating both layers;
- When deep calcified areas are detected in the myocardium, the doctor goes around their perimeter and leaves them;
- pericardial detachment is performed from the left ventricle to the left atrium, the openings of the pulmonary trunk and aorta, the right ventricle and atrium, and the openings of the vena cava;
- after excision of the pericardium, the residual edges are sutured to the intercostal muscles on the left and to the sternal edge on the right;
- The wound area is sutured layer by layer, and drains are installed for 2 days to remove fluid.
Some large clinical centers practice the method of videothoracoscopy instead of traditional pericardiectomy - cavity access with opening of the sternum. In such a situation, adhesions are separated using a laser.
Contraindications to the procedure
Pericardiectomy is a complex and largely risky operation that requires special qualifications of the operating physician and careful preliminary diagnostics. The doctor must be one hundred percent sure that the patient has no contraindications to surgical intervention.
Pericardiectomy surgery is not prescribed in the following situations:
- with myocardial fibrosis, which significantly increases the likelihood of complications and even death;
- with calcareous accumulations in the pericardial space, which are most often formed against the background of adhesive or exudative forms of pericarditis;
- in mild constrictive pericarditis.
Relative contraindications to pericardiectomy are:
- acute renal failure, as well as the chronic form of the disease;
- existing gastrointestinal bleeding;
- fever of unknown origin (possibly infectious);
- active phase of the infectious and inflammatory process;
- acute stroke;
- severe anemia;
- malignant uncontrolled arterial hypertension;
- severe electrolyte imbalances;
- severe concomitant diseases that can cause further development of complications;
- severe intoxication;
- congestive heart failure in the decompensation stage, pulmonary edema;
- complex coagulopathy.
It should be taken into account that relative contraindications are usually temporary or reversible. Therefore, pericardiectomy is postponed until the main problems that may lead to complications are eliminated.
Before surgery, the doctor evaluates the patient's condition and decides whether the operation is possible. If there are still contraindications and pericardiectomy cannot be performed, then doctors will look for other options to improve the patient's condition. [ 5 ]
Consequences after the procedure
Early postoperative consequences of pericardiectomy may include bleeding into the pleural cavity and increased cardiovascular failure. Later, purulent processes may appear in the surgical wound and purulent mediastinitis may develop. [ 6 ]
In general, pericardiectomy has a favorable prognosis. In most cases, the patient's well-being improves significantly within a month after the intervention, and cardiac activity stabilizes within 3-4 months.
Subtotal pericardiectomy has a mortality rate of 6-7%.
The main factor of mortality during surgery is considered to be the presence of previously undiagnosed myocardial fibrosis.
The main negative consequences may be:
- bleeding into the pleural space;
- arrhythmia;
- suppuration in the area of the surgical wound;
- heart attack;
- purulent form of mediastinitis;
- stroke;
- low cardiac output syndrome;
- pneumonia.
The occurrence of certain consequences of pericardiectomy may be noted depending on the patient's age, general health of the body and the cause of pericarditis. In addition, the development of complications is influenced by the anatomical features of the heart, the amount and structure of fluid in the cardiac cavity. [ 7 ]
Complications after the procedure
Despite the relatively low complication rate, pericardiectomy is an invasive procedure and is associated with certain risks. [ 8 ]
The main complications that occur during pericardiectomy are directly related to the activity of the cardiovascular system. Factors that increase the risk of complications include age, concomitant pathologies (diabetes mellitus, chronic renal failure, chronic heart failure), and multifactorial coronary circulatory disease.
Many patients complain of poor sleep, restless and even nightmares, memory loss, irritability and tearfulness, and decreased concentration for several days or weeks after pericardiectomy. Doctors say these are normal postoperative reactions that disappear on their own within the first few weeks.
Even after pericardiectomy, the patient may not immediately feel relief, but the pain will definitely go away at the end of the rehabilitation period. Pain behind the sternum may be a consequence of the process of the heart adapting to new conditions. The adaptation period is different for each patient.
The chances of improving health and quality of life after surgery must be reinforced with a combination of therapeutic exercise, drug therapy, as well as adherence to the prescribed diet and normalization of work and rest regimes. [ 9 ]
Care after the procedure
After pericardiectomy, the patient remains in hospital for about 7 days. The patient requires special observation by the doctor for 4-5 days after the operation. The first 1-2 days are spent on strict bed rest, then the activity is expanded, depending on the patient's well-being. [ 10 ]
The rehabilitation or recovery period requires compliance with the following recommendations from doctors:
- the patient must remain in bed for several days to avoid worsening the condition;
- for 1.5-2 weeks after pericardiectomy, any physical activity is contraindicated;
- until the wound is completely healed, you cannot take a bath (only a shower is allowed);
- You cannot drive vehicles during the first 8 weeks after the procedure;
- After discharge, the patient must regularly visit the attending physician, undergo control diagnostics of the cardiovascular system and general condition of the body;
- It is essential to practice therapeutic exercise – approximately 30 minutes daily, to stabilize cardiac activity;
- It is important to regularly take medications prescribed by your doctor and avoid stress and nervous tension.
In addition, an important point for recovery after pericardiectomy is adherence to special principles of dietary nutrition. Such nutrition involves limiting animal fats, salt and sugar, excluding alcoholic beverages, coffee, and chocolate. The basis of the diet should be foods that are easy to digest: vegetables and fruits, lean meat, fish and cereals. Of the drinks, green tea, rosehip infusion, and of the first courses - vegetable broths are the most useful. It is necessary to eat about six times a day, in small portions. [ 11 ]
Reviews and main questions from patients
- What is the main danger of pericardiectomy?
The average surgical mortality rate of patients undergoing pericardiectomy varies between 6-18%. The higher the qualification of the clinic, the more encouraging the statistics, which can be explained objectively. The main cause of death during pericardiectomy is considered to be the failure to detect myocardial fibrosis before surgery – a pathology for which surgical treatment is contraindicated. This is why it is very important to undergo qualified diagnostics, which allows minimizing risks both during and after surgery.
- When is it better to skip pericardiectomy?
Pericardiectomy is associated with many surgical risks, but doctors manage to minimize these risks in most cases. However, the operation is not recommended for patients with mild constriction, myocardial fibrosis, and severe pericardial calcification. The following factors increase surgical risks: patient age, renal failure.
- How long will a patient need to stay in hospital after pericardiectomy?
The rehabilitation period may vary for each patient. Most often, the patient spends the first few hours after the intervention in the intensive care unit, then he is transferred to the intensive care ward. If everything is in order, the patient is placed in a regular clinical ward, where he stays for several days until discharge.
Reviews of pericardiectomy are generally favorable. Patients report clear improvements within a month after the surgery. Cardiac activity is fully normalized within 3-4 months. It is important to note that the favorable prognosis largely depends on the experience and qualifications of the doctors and all medical personnel of the selected clinic.
After pericardial resection, the patient should regularly visit a doctor for routine examinations with a cardiologist at his place of residence, and also strictly follow the recommended preventive measures.
In general, pericardiectomy is an effective surgical operation that ensures normal heart function in conditions of impaired blood supply. The main thing is to identify the disorder in time and carry out treatment, which will eliminate the life-threatening condition of the patient.

