Methods of investigation of the autonomic nervous system
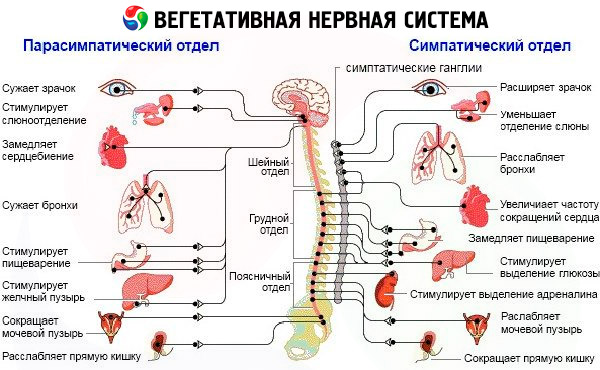
In the study of the autonomic nervous system, it is important to determine its functional state. The principles of research should be based on the clinical-experimental approach, the essence of which is the functional dynamic studies of tone, vegetative reactivity, vegetative support of activity. Vegetative tone and reactivity give an idea of the homeostatic capabilities of the organism, the vegetative provision of activity - about adaptive mechanisms. In the presence of vegetative disorders in each specific case, it is necessary to clarify the etiology and the nature of the lesion. Determine the level of damage to the autonomic nervous system : nasegmental, segmental; the primary interest of the brain structures: LRK (rynentsefalon, hypothalamus, brain stem), other cerebral structures, spinal cord; parasympathetic and sympathetic vegetative formations - sympathetic chain, ganglia, plexus, parasympathetic ganglions, lesion of sympathetic and parasympathetic fibers, namely their pre- and postganglionic segments.
Research of vegetative tone
Under the vegetative (initial) tone we mean more or less stable characteristics of the vegetative indices during the period of "relative rest", i.e. Relaxed wakefulness. In the provision of tonus, regulatory devices that support metabolic equilibrium, the relationship between sympathetic and parasympathetic systems, are actively involved.
Methods of research:
- special questionnaires;
- tables that record objective vegetative indices,
- combination of questionnaires and data of objective research of vegetative status.
Investigation of vegetative reactivity
Vegetative reactions that arise in response to external and internal stimuli characterize vegetative reactivity. In this case, the reaction force (the range of vegetative indices fluctuations) and its duration (return of vegetative indices to the initial level) is significant.
In the study of vegetative reactivity, it is necessary to take into account the "initial level law", according to which the higher the initial level, the more active and stressed state the system or organ is, the smaller the answer is possible with the action of perturbing stimuli. If the initial level is dramatically changed, then the disturbing agent can cause a "paradoxical", or antagonistic, reaction with the opposite sign, i.e., the activation value is probably related to the prestigious level.
Methods for investigating vegetative reactivity: pharmacological - introduction of a solution of adrenaline, insulin, mezaton, pilocarpine, atropine, histamine, etc .; Physical - cold and thermal samples; influence on the reflex zones (pressure): eye-cardiac reflex (Dagnini-Asnera), sino-carotid (Cermak, Goering), solar (Toma, Ru), etc.
Pharmacological tests
Method of carrying out samples with adrenaline and insulin. The study is conducted in the morning. In the horizontal position after a 15-minute rest, the subject is measured blood pressure, heart rate, etc. Subsequently, 0.3 ml of 0.1% adrenaline or insulin solution at a dose of 0.15 U / kg is injected under the skin of the shoulder. Arterial pressure, pulse, respiration are recorded after 3; 10; 20; 30 and 40 minutes after the injection of epinephrine, and after the introduction of insulin, the same values are recorded every 10 minutes for 1.5 hours. For changes in systolic and diastolic pressure we took its fluctuations exceeding 10 mm Hg. For the change in heart rate - an increase or decrease by 8-10 or more strokes per minute, respiration by 3 or more per 1 minute.
Evaluation of samples. Three degrees of vegetative reactivity are distinguished: normal, elevated, lowered. In the group of healthy persons it was found:
- no response to the introduction of a pharmacological substance in 1/3 of the examined;
- a partial (weak) vegetative reaction, characterized by a change in one or two objective indicators (blood pressure, pulse or respiration), sometimes in combination with mild subjective sensations or a change in three objective indicators without subjective sensations - in 1/3 of the examined;
- a pronounced (increased) vegetative reaction at which all three registered objective indicators change in combination with the manifestation of subjective complaints (palpitations, chills, feelings of inner tension or, conversely, weakness, drowsiness, dizziness, etc.) - 1 / 3 of the examined.
Depending on the nature of the vegetative shifts and subjective sensations, sympathoadrenal reactions are identified, vagoinsular, mixed, biphasic (in the latter, the first phase may be sympatoadrenal, and the second - parasympathetic or vice versa).
Physical exercise
Methods of conducting a cold sample. In the prone position, blood pressure and heart rate are measured. Then the examinee drops the wrist of the other hand to the wrist in the water, the temperature of which is +4 ° C, and holds 1 minute, while the blood pressure and heart rate are recorded immediately after immersion of the brush in water, 0.5 and 1 min after immersion, and then - after the hand is taken out of the water - blood pressure and heart rate are recorded before coming to the initial level. If the heart rate is examined by ECG, the number of R teeth or RR intervals is counted into the indicated time intervals and all are recalculated to a heart rate of 1 min.
Evaluation of the sample. Normal vegetative reactivity is an increase in systolic blood pressure by 20 mm Hg. St, diastolic - by 10-20 mm Hg. Art. In 0.5-1 minutes. Maximum rise in blood pressure - after 30 seconds after the start of cooling. Return of blood pressure to baseline - after 2-3 min.
Pathological abnormalities:
- superexcitability of vasomotors (hyperreactivity) - a strong increase in systolic and diastolic blood pressure, ie, a pronounced sympathetic reaction (increased vegetative reactivity);
- a decrease in the excitability of the vasomotors (hyporeactivity) - a slight rise in blood pressure (an increase in diastolic pressure of less than 10 mm Hg), a weak sympathetic response (reduced autonomic reactivity);
- decrease in systolic and diastolic pressure - parasympathetic reaction (or perverted reaction).
Pressure on the reflex zones
Eye-reflective reflex (Dagnini-Asnera). Technique of the sample: after a 15-minute resting, ECG is recorded for 1 minute with further calculation of the heart rate for 1 min (initial background). Then pads of fingers pressed on both eyeballs until a slight painful sensation appeared. It is possible to use Barre's okulokompressor (pressure 300-400 g). After 15-25 seconds after the start of the pressure, ECG is recorded for 10-15 seconds. Count the number of teeth R for 10 seconds and count for 1 minute.
You can record the heart rate after stopping the pressure for another 1-2 minutes. At this heart rate, a percentage increase in the RR interval during the last 10 seconds of pressure on the eyeballs is taken against the average value of the RR intervals calculated in the five 10-second intervals RR before the start of the pressure.
You can also read the heart rate not according to the ECG record, but palpation every 10 seconds for 30 seconds.
Interpretation: normal retardation of heart rate - normal vegetative reactivity; severe retardation (parasympathetic, vagal reaction) - increased autonomic reactivity; low retardation - decreased autonomic reactivity; absence of deceleration - perverted vegetative reactivity (sympathetic reaction).
Normally, after a few seconds from the start of the pressure, the heart rate slows down in 1 minute increments by 6-12 strokes. The ECG determines the slowing of the sinus rhythm.
All the estimates of the samples indicate both the strength and the nature of the reaction. However, the digital data obtained from the examination of healthy people are not the same for different authors, probably due to a number of reasons (different initial heart rate, different recording and processing methods). In connection with the different initial heart rate (more or less than 70-72 beats per minute), a Galya formula can be calculated:
Х = Heart rate / heart rate x 100,
Where ЧССп - heart rate in the sample; Heart rate - the initial heart rate; 100 - conditional number of heart rate.
The slowing of the pulse according to Galya's formula is: 100 - X.
For the norm, we consider it expedient to take the value M ± a, where M is the average HR value in 1 min in the study group; o - root-mean-square deviation from M. At a value higher than M + g, one should speak about increased vegetative reactivity (sympathetic or parasympathetic), with a value lower - about decreased vegetative reactivity. We consider it necessary to carry out the calculation in this way and with other samples for vegetative reactivity.
Results of the study of heart rate in samples in healthy individuals
|
Try |
M ± a |
|
Eye reflex |
-3.95 ± 3.77 |
|
The sinocarotid reflex |
4.9 ± 2.69 |
|
The solar reflex |
-2.75 ± 2.74 |
The sino-carotid reflex (Cermak-Goering). Technique of the sample: after 15 minutes of adaptation (rest) in the prone position, the heart rate is counted in 1 min (ECG record - 1 min) - the initial background. Then alternately (after 1,5-2 s) with your fingers (forefinger and large) press on the area of the upper third of m. Sternoclaidomastoideus slightly below the angle of the lower jaw to a sensation of pulsation of the carotid artery. It is recommended to start the pressure on the right side, since the irritation effect on the right is stronger than on the left. The pressure should be light, not causing pain, for 15-20 seconds; from the 15th second they begin to register the heart rate with the help of ECG for 10-15 seconds. Then the pressure is stopped and the frequency of the R- wave ECG counts the heart rate in min. You can calculate by the value of the RR interval , as well as in the study of the eye-cardiac reflex. It is possible to record the state of aftereffect at the 3rd and 5th minutes after the pressure ceases. Sometimes they record blood pressure, respiratory rate.
Interpretation: for normal changes in heart rate take the values obtained in healthy subjects, ie, normal vegetative reactivity.
The values above this testify to increased vegetative reactivity, ie, increased parasympathetic or insufficiency of sympathetic activity, and lower - to a decrease in vegetative reactivity. Strengthening the heart rate indicates a perverse reaction. According to the data of other authors [Rusetsky II, 1958; Birkmayer W., 1976, etc.), the norm is the slowing down of the heart rate after 10 s to 12 strokes per minute, the reduction in arterial pressure to 10 mm, the slowing of the respiratory rate, sometimes the rise of the T wave on the ECG by at least 1 mm.
Pathological abnormalities: sudden and significant deceleration of heart rate without falling of arterial pressure (vagocardial type); a strong drop in blood pressure (above 10 mm Hg) without slowing the pulse (depressor type); dizziness, fainting without changes in blood pressure or pulse, or with changes in these parameters (cerebral type) - lifting of blood pressure (Birkmayer W., 1976). Therefore, it is expedient to calculate the values of M ± a.
The solar reflex is the epigastric reflex (Toma, Ru). Technique of the sample: at rest in a supine position with relaxed abdominal muscles, the ECG is recorded before the sample (background), the RR ECG intervals determine the heart rate. It is possible to investigate and arterial pressure (parameters of an initial background). The pressure on the solar plexus is made by hand to a sensation of pulsation of the abdominal aorta.
At the 20-30th second from the beginning of the pressure, the heart rate is recorded again for 10-15 seconds with the help of an ECG. The heart rate is counted by the number of teeth R on the ECG for 10 s and counted for a minute. The calculation can be made according to the value of the RR interval as well as in the study of the eye-cardiac reflex (see above).
Interpretation: the norm is taken to be M ± o. Determine the degree of severity - normal, increased or pronounced, reduced and distorted reactivity and the nature of the reaction - sympathetic, vagal or parasympathetic.
According to the data of II Rusetskii (1958), W. Birkmayer (1976), several types of reaction are noted:
- the reflex is absent or inverted (the pulse is not sufficiently slowed down or more frequent) - a sympathetic type of reaction;
- reflex positive - slowing down more than 12 beats per 1 min - parasympathetic type;
- slowing down by 4-12 beats per minute - the normal type.
When testing for reactivity, you can calculate the coefficients indicated in the study of the vegetative tone. The results obtained from the samples give an idea of the strength, nature, duration of vegetative reactions, ie, the reactivity of the sympathetic and parasympathetic divisions of the VNS.
Research of vegetative maintenance of activity
The study of vegetative maintenance of various forms of activity also carries important information about the state of the autonomic nervous system, since vegetative components are a compulsory accompaniment of any activity. Registration of them we call research of vegetative maintenance of activity.
The indices of vegetative maintenance allow to judge about adequate vegetative maintenance of behavior. In norm it is strictly correlated with form, intensity and duration of action.
Methods of research of vegetative maintenance of activity
In clinical physiology, the study of vegetative maintenance is performed using experimental activity modeling:
- physical - dosed physical exercise: veloergometry, dosed walking, lifting legs lying in a horizontal position by 30-40 ° a certain number of times for a certain period of time, a two-stage trial of the Master, metered squats, dynamometer press up to 10-20 kg, etc .;
- sample position - transition from horizontal to vertical position and vice versa (orthoclinostatic test);
- mental - account in the mind (simple - subtract from 200 to 7 and complex - multiplication of two-digit numbers by double-digit), composing words, for example 7 words of 7 letters, etc .;
- emotional - simulation of negative emotions: the threat of electric shock, the reproduction of negative emotional situations experienced in the past, or the special evocation of negative emotions associated with the disease, the development of emotional stress through the Kurt Levine method, etc. Simulation of positive emotions in different ways, for example, a good outcome of the disease, etc. To register vegetative shifts, the parameters of the cardiovascular system are used: heart rate, PC variability, ION, REG indicators, plethysmography, and so on. Etc .; respiratory system - respiratory rate, etc .; the skin-galvanic reflex (GSR), the hormonal profile and other parameters are examined.
The investigated indicators are measured at rest (the initial vegetative tone) and in the performance of the activity. The increase in the indicator during this period is estimated as the II vegetative support of activity. Interpretation: the data obtained are interpreted as normal vegetative maintenance of activity (shifts are the same as in the control group), excessive (shifts are more intense than in the control group), insufficient (shifts are less pronounced than in the control group).
The provision of activities is carried out mainly by an ergotrope system. Therefore, the degree of deviation from the initial data was judged on the state of the ergotropic apparatus.
Investigation of vegetative maintenance in the orthoclinostatic sample. This test is described by many authors [Rusetsky II, 1958; Chetverikov N. S, 1968, etc.] and has several modifications based on the hemodynamic Schölong trial. We will give only two of its variants. The first variant (classical) is described in the manual by W. Birkmayer (1976); The second variant, which we adhere to recently, is the sampling and processing of the results obtained using the method proposed by Z. Servit (1948).
Ortlin-static tests conducted actively, and not by means of a turntable, we regard not only as hemodynamic, but also as tests for vegetative support of activity, ie, vegetative shifts that ensure the transition from one position to another, and then the maintenance of a new position .
The methodology of the first option. At rest and horizontal position, heart rate and blood pressure are determined. Then the patient slowly, without unnecessary movements, gets up and in a comfortable position stands near the bed. Immediately in a vertical position, the pulse and blood pressure are measured, and then it is done at minute intervals for 10 minutes. In the vertical position, the subject may be between 3 and 10 minutes. If pathological changes appear at the end of the sample, the measurement should continue. The patient is asked to lie down again; immediately after stowing are measured at minute intervals of blood pressure and heart rate until they reach the initial value.
Interpretation. Normal reactions (normal vegetative maintenance of activity): on rising - a short-term rise in systolic pressure up to 20 mm Hg. St., to a lesser degree diastolic and transient increase in heart rate to 30 in 1 min. During standing, systolic pressure may sometimes drop (by 15 mm Hg below the baseline level or remain unchanged), the diastolic pressure invariably or slightly rises, so that the pressure amplitude against the initial level may decrease. The heart rate during the standing can increase to 40 in 1 min against the initial. After returning to the starting position (horizontal), blood pressure and heart rate should come to the initial level in 3 minutes. Immediately after laying, a brief rise in pressure may occur. There are no subjective complaints.
Violation of the vegetative support of the activity is manifested by the following signs:
- Elevation of systolic pressure by more than 20 mm Hg. Art.
- Diastolic pressure is also increased, sometimes more significantly than systolic pressure, in other cases it falls or stays at the same level;
- Self-elevation only diastolic pressure when rising;
- Increase in heart rate on rising more than 30 in 1 min;
- At the time of getting up, there may be a sensation of a rush of blood to the head, a darkening in the eyes.
All the above changes indicate excessive vegetative maintenance.
- The transient drop in systolic pressure by more than 10-15 mm Hg. Art. Immediately after getting up. The diastolic pressure can simultaneously increase or decrease, so that the pressure amplitude (pulse pressure) decreases significantly. Complaints: rocking and feeling weak at the moment of getting up. These phenomena are treated as insufficient vegetative maintenance.
- During standing, the systolic pressure drops by more than 15-20 mm Hg. Art. Below the original level. The diastolic pressure remains unchanged or slightly rises - a hypotonic disorder of regulation, which can also be regarded as insufficient vegetative maintenance, as a violation of adaptation. Similarly, the drop in diastolic pressure (hypodynamic regulation according to W. Birkmayer, 1976) can also be assessed. Reduction of the amplitude of arterial pressure in comparison with the initial level more than 2 times signifies not only regulatory violations, but, in our opinion, a violation of vegetative provision.
- Increased heart rate during standing by more than 30-40 in 1 min with relatively constant arterial pressure - excessive vegetative maintenance (tachycardic regulatory disorder according to W. Birkmayer, 1976). Orthostatic tachypnea may occur.
ECG changes in the orthoclinostatic test: an increase in the sinus pulse frequency, an increase in the P wave in the II and III standard leads, a decrease in the ST interval and a flattening or negative T wave in the II and III leads. These phenomena can occur either immediately after rising, or with prolonged standing. Orthostatic changes can be observed in healthy individuals. They do not indicate a cardiac defect: this is a violation of the vegetative provision associated with sympathicotonia - excess supply.
To go to a recumbent position and in a recumbent position, the rules are the same.
The methodology of the second option. After 15 minutes of rest, the blood pressure is measured in a horizontal position, the heart rate is recorded by recording the ECG for 1 minute. The examinee quietly ascends to a vertical position, which takes about 8-10 seconds. After that, in the vertical position again for 1 minute continuously recorded ECG, recorded blood pressure. In the future, at the 3rd and 5th minutes of the stand, ECG is recorded for 20 s and blood pressure is measured during the same time intervals after ECG recording. Then the examinee lies down (clenostatic test), and again register the same vegetative indices according to the method described above in the same time intervals. The heart rate is recorded by counting the R teeth in 10-second intervals of the ECG.
The processing of the data obtained over a minute interval of orthostatic and clinostatic samples is carried out according to Z. Servit (1948). The following indicators are calculated:
1. Average orthostatic acceleration in 1 min (SDA). It is equal to the sum of the gain relative to the initial heart rate in the first 10-second minute, second and sixth, divided by 3:
СОУ = 1 + 2 + 6/3
Orthostatic Lability Index (OIL) - the difference between the highest and lowest HR in the orthostatic position for 1 min (selected from six 10-second intervals of the first minute) - the minimum range of heart rate fluctuations in the orthostatic sample.
Klinostatichesky slowing (CP) - the greatest slowdown in heart rate for 1 min in the supine position after a transition from a vertical position.
The orthoclinostatic difference (OCD) is the difference between the greatest acceleration and the greatest deceleration in the ortho- and clinostatic sample (calculation is also performed for six 10-second intervals in 1 minute of the sample).
The klinostatic lability index (CIL) is the difference between the largest and the smallest heart rate slowdown with a clinostatic sample (selected from 10-second intervals of 1 minute horizontal position). The entire calculation is carried out within 1 minute in the standing and lying position, and then the heart rate is calculated on the 3rd and 5th minutes and the blood pressure value. The values of M ± a, obtained from healthy specimens tested at various intervals of time, are taken as the norm.
Dynamic study of the vegetative nervous system gives an idea of its initial vegetative tone (determined by the state of peripheral vegetative formations), autonomic reactivity, vegetative support of activity, which is caused by the state of superegmental brain systems that organize adaptive behavior.
In addition to the above-described functionally dynamic method, widely used by clinicians with the registration of these parameters for the characteristic of the state of the vegetative nervous system at rest and under loads, REG is used which gives indirect information about the magnitude of pulse blood filling, the state of the vascular wall of the main vessels, the relative velocity of blood flow, and venous circulation. Those tasks are solved with the help of plethysmography: an increase in the oscillation, that is, dilatation of the vessels, is regarded as a decrease in sympathetic influences; The decrease in oscillations, the tendency to constriction - as their amplification. Ultrasonic dopplerography (UZDG) testifies to the state of the vascular bed, which also indirectly reflects the state of the autonomic nervous system.
Study of neuromuscular excitability
The following objective tests are most often used.
Evoke the symptom of Khvostek at rest and after a 5-minute hyperventilation. The development of the symptom of the tail is performed by striking the neurological malleus at a point along the midline connecting the corner of the mouth and the earlobe. The degree of severity is measured:
- I degree - reduction of labial commissure;
- II degree - joining the contraction of the wing of the nose;
- III degree - in addition to the phenomena described above, the ocular muscle of the eye contracts;
- IV degree - a sharp contraction of the muscles of the entire half of the face.
Hyperventilation for 5 minutes leads to a distinct increase in severity [Alajouianine Th. Et al., 1958; Klotz HD, 1958]. Among healthy people, a positive symptom of hvostec occurs in 3-29%. In neurogenic tetany, it is positive in 73% of cases.
Cuff test (symptom of Tissot). Technique: an arterial tourniquet or pneumatic cuff is applied to the subject's shoulder for 5-10 minutes. The pressure in the cuff should be maintained at 5-10 mm Hg. Art. Higher than the patient's systolic pressure. With the removal of compression in the postischemic stage, there are carpopedic spasms, the phenomenon of "obstetrician hands". The frequency of the Tissot symptom in tetany varies from 15 to 65%. It indicates a high level of peripheral neuromuscular excitability.
Trusso-Bonsdorf Trial. Technique: an air cuff is placed on the subject's shoulder and the pressure is maintained for 10-15 mm Hg within 10 minutes. Art. Higher than the systolic pressure of the patient, which causes ischemia of the hand. In the second half of the ischemic period, hyperventilation (maximum deep breaths and expirations with a frequency of 18-20 per 1 min) is added during 5 minutes. Sample results: weakly positive - the appearance of visible fasciculations in the interstitial muscles, especially in the region of the I interphalangeal interval, the change in the shape of the hand (the tendency to the emergence of the "hand of an obstetrician"); positive - a pronounced picture of carpopedic spasm; negative - the absence of the phenomena described above.
Electromyographic study. When EMG-study recorded a certain type of electrical activity of the muscles involved in tetanic spasm. The activity is characterized by consecutive potentials (doublets, triplets, multiplets) that occur during short time intervals (4-8 ms) at a frequency of 125-250 cps. Such potentials and other phenomena in EMG arise during the study period with the help of provocative samples.
Other tests that detect neuromuscular excitability: Bechterew's ulnar syndrome, Schlesinger's symptom, a symptom of a muscular cushion, but they are less informative and less common.
Methods for the study of hyperventilation syndrome
- Analysis of subjective feelings (complaints), characterized by polysystem and the connection of complaints with respiratory function.
- The presence of respiratory disorders during or at the onset of the disease.
- Positive results of a hyperventilation test.
- Samples for neuromuscular excitability.
- The possibility of arresting hyperventilation paroxysm by inhaling an air mixture containing 5% CO2, or breathing "into a bag" (paper or polyethylene) to accumulate its own CO2, by which an attack is arrested.
- The patient has hypocapnia in the alveolar air and alkalosis in the blood.
The technique of conducting a hyperventilation test: the patient is in a horizontal position or a reclining position (in the chair). Begins to breathe deeply with a frequency of 16-22 breaths in 1 min. The sample lasts depending on the tolerance from 3 to 5 minutes. A positive hyperventilation test has two variants of percolation. The first variant: during the test period there are emotional, vegetative, tetanic and other changes that disappear after 2-3 minutes after its termination. The second option: hyperventilation leads to the development of autonomic paroxysm, which, starting during the test, continues after its termination. The passage of the sample into the unfolded paroxysm is first observed in the breath, the subject can not stop hyperventilation and continues to breathe deeply and often. Disturbance of breathing is accompanied by vegetative, muscular-tonic and emotional disorders. It is generally believed that the emergence during the trial of subjective sensations that resemble spontaneous emergence is a positive criterion for establishing a diagnosis of hyperventilation syndrome.
At the age of over 50 years, it is necessary to carry out the test carefully. Contraindications are high blood pressure, the presence of cardiac and pulmonary pathology, pronounced atherosclerosis.
Additional methods for studying the functional state of the nervous system
Investigation of emotional and personal characteristics
Vegetative disorders, especially the cerebral level, are psycho-vegetative. Therefore, in vegetative disorders it is necessary to investigate the psychic sphere. One of the methods of its study is a detailed study of psychoanalysia, iotirovanie the availability of children and urgent psychotrauma. Clinical analysis of emotional disorders is important. Psychological examination is carried out with the help of various methods: the method of multifaceted personality research (MIL) in the modification of FB Berezin and Miroshnikov (1976), the tests of Spielberger, Eysenck, Cattell, and the Rorschach project test, the thematic apperceptive test (TAT ), the test of unfinished sentences, the Rosenzweig test (frustration test), etc. The most informative in the study of autonomic disorders are the tests of MIL, Spielberger, Cattel.
Electrophysiological studies
EEG is used not only to clarify the localization of the process and, in some cases, its character (epileptic hypersynchronous generalized discharges), but also to study the functional state of nonspecific activating and deactivating brain systems in sleep, in relaxed and intense wakefulness, which is modeled by various loads: hyperventilation, light, sound stimulation, emotional stress, mental stress, etc.
The most common method for testing nonspecific brain systems is the polygraph registration of EEG, ECG, RG, EMG, respiratory rate. Shifts of these indicators reflect the relationship between the ascending and descending activating system-Mi. The ratio and state of desynchronizing (reticular formation of the brainstem) and synchronizing (thalamocortical system) of brain systems are judged by visual and computer analysis of EEG (calculation of a-index, current synchronization index, etc.). During the sleep period, EEG data provide information on the characteristics of the representation of various stages of sleep, their latent periods, sleep cycles and motor activity (AID).
In recent years, the use of computer technology has significantly increased the possibilities of neurophysiological research. Using the averaging method, it was possible to isolate from the spontaneous EEG potential-related potentials, mainly caused by sensory and motor stimuli.
Thus, the study of somatosensory evoked potentials makes it possible to evaluate effectively and differentially the functional state of different levels of specific and nonspecific afferentation systems.
The study of the mechanisms of the organization of action and effector systems makes it possible to register motor potential associated with arbitrary movements and reflecting both the overall processes of organizing actions and decision-making, and more local mechanisms for activating cortical motor neurons.
Registration of contingent negative deviation (CCW) is used to study the mechanisms of directional attention, motivation, probabilistic prediction, which allows us to evaluate the state of nonspecific brain systems.
The study of the peculiarities of the mechanisms of topographic organization of brain activity is possible using the construction of spectral maps of spontaneous EEG.
Compressed spectral analysis (CSA) using the Fast Fourier Transform algorithm allows to determine the spectral power of EEG rhythms and their reactivity to various functional loads, which also provides information on the state of nonspecific brain systems. In addition, CSA EEG reveals the character of interhemispheric interaction (interhemispheric asymmetry) involved in adaptive reactions.
Study of hormonal and neurohumoral functions
Often, vegetative disorders are combined with neuro-endocrine-metabolic disorders. They are based on changes in neurohormonal and neurohumoral relationships (due to the change in neurotransmitter mediation), which, in turn, are indicators of the adaptive capabilities of the body and the state of ergo- and trophotropic systems.
In a number of cases it is necessary to investigate both the hormonal profile and the neurohumoral relationships: the thyroid function (the main metabolism using the complex radioisotope absorption method I), the state of the hypothalamus-pituitary-adrenal cortex system (the determination of corticosteroids and their metabolites in blood and urine), the examination functions of the ovaries (rectal temperature, pupil symptom, CII, hormonal profile), carbohydrate, protein, water-salt metabolism, etc.
In order to study the state of neurohumoral relationships, the content of catecholamines (adrenaline, noradrenaline, dopamine, DOPA and their metabolites), acetylcholine and its enzymes, histamine and its enzymes (diaminoxidase), the histamine-retardation effect of serotonin by excretion are determined in the blood, urine, cerebrospinal fluid with urine 5-OIUK.
At the same time, these indicators can be used to assess the state of both specific and non-specific LRC systems, as well as reactions of central ergo- and trophotropic devices and peripheral vegetative systems.
Humoral (electrolyte) studies of sodium, potassium, total calcium, inorganic phosphorus, chlorine, carbon dioxide, magnesium contribute to the release of latent neurogenic tetany. The coefficients indicating the ratio of monovalent ions (sodium, potassium) to bivalent ions (calcium, magnesium) are determined. Syndrome of neurogenic tetany (SNT) is mainly normocalcemic, but there is a relative tendency to hypocalcemia. Patients with SNT significantly increased the coefficient reflecting the predominance of monovalent ions over bivalent ones.
Research of the functions of the segmental department of the autonomic nervous system
The development of modern teaching on the pathology of the autonomic nervous system required a revision of old methodological approaches and the development of new research methods. Today, special methods are being applied to the methods being developed. Tests for vegetative studies should be:
- sufficiently informative regarding autonomic dysfunction (quantitative evaluation of the results);
- specific, with well-reproducible results in repeated studies (the coefficient of variation should not exceed 20-25%); 3) physiologically and clinically reliable (safe);
- non-invasive;
- easy and fast.
There are still few tests that meet these requirements.
The methods developed for the study of the autonomic nervous system in cardiovascular, shipmotor and pupillary systems are more likely than others to meet the above requirements and therefore enter clinical practice more quickly.
The study of segmental vegetative disorders should be carried out taking into account not only the localization of the lesion, but also the symptoms that indicate the loss or irritation of peripheral vegetative formations. If possible, determine their character (sympathetic or parasympathetic). It is desirable at the same time to clarify the interest of a certain part of the autonomic arc: afferent or efferent.
Some of the methods used can provide information on supra-segmental vegetative devices, registering the initial vegetative tone, vegetative reactivity and vegetative maintenance of activity, in addition, one can obtain information about the state and segmental parts of the autonomic nervous system.
The cardiovascular system
Methods for determining the state of the sympathetic efferent pathway
- Determination of changes in blood pressure associated with the transition to the vertical position. Calculate the difference in systolic blood pressure in the prone position and in the 3 rd minute after rising.
Interpretation: a systolic blood pressure drop of no more than 10 mm Hg. Art. - a normal reaction, indicating the intactness of efferent vasoconstrictor fibers; a fall of 11-29 mm Hg. Art. - Border reaction; a drop of 30 mm Hg. Art. And more - a pathological reaction, indicating an efferent sympathetic failure.
- Determination of changes in blood pressure under isometric loading. Using a dynamometer, determine the maximum force in one hand. Then for 3 minutes. The patient compresses the dynamometer with a force equal to 30% of the maximum. Calculate the difference in diastolic blood pressure at the 3rd minute of the dynamometer compression and before the exercise, at rest.
Interpretation: increased diastolic blood pressure by more than 16 mm Hg. Art. - normal reaction; an increase of 10-15 mm Hg. Art. - Border reaction; increase by less than 10 mm Hg. Art. - pathological reaction, indicating the efferent sympathetic failure.
- Assessment of the state of efferent vasoconstrictive sympathetic fibers. To do this, use some samples based on the registration plethysmogram of the hand or forearm:
- presentation of mental load, pain stimulus or sudden noise causes a normal decrease in the blood filling of the hand and an increase in blood pressure due to peripheral vasoconstriction. The absence of changes in blood filling and arterial pressure testifies to the defeat of efferent sympathetic fibers reaching the vessels of the skin;
- on carrying out the Valsalva test or a rotational test in the Barani chair, the blood filling decreases normally due to the enhancement of vasoconstriction. The absence of changes in blood filling testifies to the defeat of sympathetic peripheral vasoconstrictors;
- a sharp deep breath causes a reflex narrowing of the vessels of the forearms. With this sample, the reaction is based on a spinal reflex, whose afferent ways are unknown, and the efferent pathways consist of sympathetic vasoconstrictor fibers. The absence of a decrease in blood filling with this sample also indicates sympathetic efferent insufficiency;
- with sit-ups, passive raising of the legs in the supine position on the plethysmograph, there is an increase in blood filling due to a reduction in vasoconstriction. With the defeat of sympathetic vasoconstrictor fibers reaching the vessels of the skeletal musculature, there are no changes in blood filling.
It should be noted that these samples using plethysmography do not have clear quantitative limits of the norm and pathology, and therefore their use in general practice is limited. However, the results obtained in the group of subjects can be compared with the data of the control group.
- Pharmacological tests:
- determination of the level of norepinephrine (NA) in plasma: the concentration of norepinephrine in the blood plasma is maintained by releasing it from the sympathetic nerve endings and the medulla of the adrenal glands. Considering that the amount of the neurotransmitter released into the blood is proportional to the activity of the sympathetic nervous system, the plasma norepinephrine concentration can be used as an index of sympathetic nervous activity. It is suggested that a decrease in noradrenaline content in the blood plasma is more likely a consequence of pathological isolation of it from the sympathetic efferent terminals of blood vessels than the result of changes in its capture or diffusion through the blood-brain barrier or other membranes. In a healthy person in a prone position, the plasma norepinephrine level remains at a constant level and sharply increases when going to the vertical position. At the central positions of the autonomic nervous system there is a certain level of norepinephrine in the plasma, which does not change during the transition to the vertical position. With peripheral lesions (postganglionic sympathetic neuron), the level of norepinephrine in the supine position is sharply reduced and does not increase with orthotest. Thus, it is possible to differentiate preganglionic lesion from postganglionic lesion:
- test with tyramine: tyramine releases norepinephrine and dopamine from postganglionic presynaptic vesicles. Insufficient increase in noradrenaline (catecholamines) of plasma after administration of tyramine will indicate an inadequate ability of postganglionic neuron to release noradrenaline, i.e., a distal postganglionic sympathetic defect;
- a test with norepinephrine: intravenous administration of small doses of norepinephrine causes a healthy person a large number of cardiovascular effects, including an increase in systemic blood pressure. In some patients with vegetative lesions, there is an exaggerated response of arterial pressure due to the so-called denervation hypersensitivity arising during the destruction of presynaptic nerve endings. Conversely, complete denervation leads, with this sample, to a lower blood pressure response than normal;
- test with anaprilin: no slowing of heart rate with intravenous injection of anaprilin (no more than 0.2 mg / kg) indicates the defeat of sympathetic nerves going to the heart.
- Registration of the action potentials of the sympathetic peripheral nerves going to the vessels of the skin, the striated muscle and to the sweat glands. The modern electrophysiological method that allows using new microelectrode techniques to register neuronal activity from peripheral vegetative nerves, to determine latent periods of vegetative responses for different types of stimuli, and to calculate the rate of excitation of efferent sympathetic fibers.
Methods for determining the state of the parasympathetic efferent pathway
- Changing heart rate on rising. In healthy people, the heart rate rises quickly when you get up (the maximum number is recorded after the 15th stroke of heart beat) and then decreases after the 30th stroke. The ratio between the RR interval at the 15th strike and the RR interval at the 30th strike is referred to as "30: 15 ratio" or "30: 15" ratio. In norm it is equal to 1.04 and more; 1,01-1,03 - borderline result; 1,00 - insufficiency of the vagal effects on the heart.
- Changing the heart rate with deep, slow breathing - 6 times in 1 min. Determination of the relationship of the maximally extended cardio interval RR during expiration to the maximally shortened RR interval during inspiration. In healthy people due to sinus arrhythmia, due to the influence of the vagus, this ratio is always greater than 1.21. Indicators 1.11-1.20 are borderline. With decreasing sinus arrhythmia, i.e. In case of vagus failure, the indicated index will not be higher than 1.10.
- Change in heart rate with a Valsalva test. Calculate the Valsalva coefficient. Breathing is done in the mouthpiece, connected to a manometer; the pressure is maintained at 40 mm Hg. Art. Within 15 seconds. At the same time, heart rate is recorded with ECG. Calculation of the Valsalva coefficient: the ratio of the extended RR interval in the first 20 seconds after the sample to the shortened RR interval during the sample. In norm it is equal to 1.21 and more; border outcomes - 1.11-1.20; a factor of 1.10 or lower indicates a violation of parasympathetic regulation of the rhythm of the heart. Physiologically, during the test at the time of stress, there is tachycardia and vasoconstriction, after which there is a jump in blood pressure and later there comes a bradycardia.
- Pharmacological tests:
- test with atropine. Complete cardiac parasympathetic blockade occurs when atropine is administered at a dose of 0.025-0.04 mg / kg, respectively, from 1.8 to 3 mg of atropine sulfate. The effect is achieved within 5 minutes, lasts 30 minutes. There is severe tachycardia. In patients with cardial branches of the vagus, there is no increase in heart rate.
Methods for determining the state of the afferent sympathetic pathway
Valsalva test: breathing is carried out into a mouthpiece connected to a manometer; The pressure in the manometer is maintained at 40 mm Hg. Art. Within 15 seconds.
This increases the intrathoracic pressure, changes blood pressure and heart rate. All changes in the norm last 1.5-2 minutes and have four phases: 1-st phase - increase in blood pressure due to increased intrathoracic pressure; 2-nd phase - a drop in systolic and diastolic pressure due to a change in the venous inflow; After 5 seconds the blood pressure level is restored, which is associated with reflex vasoconstriction; The heart rate rises in the first 10 seconds; 3-rd phase - a sharp drop in blood pressure to the level of the end of the 2 nd phase, which is associated with the release of the aorta; this condition lasts 1-2 seconds after the disappearance of intrathoracic pressure; The 4th phase - raising the systolic pressure above the resting level for 10 s, the pulse pressure increases, the diastolic pressure either rises or does not change. The 4th phase ends when the arterial pressure returns to the original level.
When the sympathetic afferent path is affected, blockade of the response occurs in the 2 nd phase, which is manifested by a drop in systolic and diastolic pressure and an increase in heart rate.
If it is known that the vagus nerve is functioning normally (according to clinical data and the results of the tests) and there is no change in heart rate with arterial hypo- and hypertension, it can be assumed that the afferent part of the sympathetic arch has suffered, i.e., the path leading to carotid sinus in the IX pair of cranial nerves.
Modern methods of research of vegetative apparatuses in the cardiovascular system are non-invasive monitoring of arterial pressure and analysis of variability of the heart rhythm (PC spectral analysis). These methods allow to give an integrative quantitative evaluation of the vegetative function in various functional states, to clarify the influence and role of the sympathetic and parasympathetic links of vegetative regulation in the cardiovascular system.
Gastrointestinal system
The methods used to study vegetative functions in this system are based on a study of the motility of the entire gastrointestinal tract, which is under the control of the parasympathetic and sympathetic parts of the autonomic nervous system.
Before proceeding to the description of methods, it is necessary to warn that positive results can be interpreted as a vegetative pathology in the event of the exclusion of all the obvious causes of gastrointestinal disorders (infection, inflammation, trauma, tumor, adhesion, liver and gallbladder pathology, etc.). ).
Exercise of excretory function. Methods for determining the state of the parasympathetic efferent pathway
- Acidity of gastric juice. Enter insulin - 0,01 ED / kg with the subsequent determination of acidity of gastric juice. In a healthy person in response to the onset of hypoglycemia due to the activity of the vagus nerve increases acidity. The absence of an increase in acidity indicates the damage to the branches of the vagus going to the parietal cells of the stomach. By the way, this is the standard procedure for evaluating surgical vagotomy. If parietal cells are affected or absent, then in response to pentagastrin or histamine there will also be an increase in the acidity of the gastric juice.
- Gastrochromoscopy. It is based on the ability of the gastric mucosa to release the paint - neutral red - after 12-15 minutes with intramuscular injection and after 5 minutes with intravenous injection. With secretory deficiency, the secretion of the paint is significantly delayed, with achilia - it does not occur at all (the predominance of sympathetic influence).
- The reaction of pancreatic polypeptides to hypoglycemia. The release of pancreatic polypeptides from the pancreas occurs during hypoglycemia and is mediated by the vagus. On this basis, insufficient or no increase in pancreatic polypeptides in response to the administration of insulin is regarded as a parasympathetic insufficiency.
Study of motor and evacuation function of the stomach and intestines
The methods described indicate the defeat of preganglionic parasympathetic fibers or sympathetic failure.
Methods: scintigraphy, roentgenography, manometry. It is possible to detect a delay in the movements of the esophagus that occurs when the preanglionic parasympathetic fibers of the vagus nerve are damaged, and the rhythm of movements in axonal degeneration of the esophagal nerves is disturbed.
Contrastive methods of studying the stomach and intestines, electrogastrography, ultrasonography can detect violations of motor function in the form of slowing of peristalsis and evacuation in parasympathetic nerves (vagus) and motor stimulation with sympathetic failure.
- Balloon-kymographic method. The essence lies in the registration of intragastric pressure, the fluctuations of which largely correspond to the contractions of the stomach. The initial level of pressure characterizes the tone of the walls of the stomach. An air filled rubber cylinder is connected through a system of tubes and a Marey capsule with a water manometer. Fluctuations in the liquid in the manometer are recorded on the kymograph. When analyzing kymograms, the rhythm, the strength of the gastric contractions, and the frequency of peristaltic waves per unit time are evaluated. Effects that go along sympathetic nerves, reduce the rhythm and force of contraction, as well as the rate of distribution of the peristaltic wave along the stomach, inhibit motility. Parasympathetic influences stimulate motility.
- The method of open catheters is a modification of the balloon-kymographic method. The pressure in this case is perceived by the meniscus of the liquid.
- Electrogastrography has the advantages of a no-probe method for assessing gastric motility. The biopotentials of the stomach are recorded from the patient's body surface with the help of EGG-3, EGG-4. The system of filters allows us to identify biopotentials in a narrow range, characterizing the motor activity of the stomach. When assessing gastrograms take into account the frequency, rhythm, amplitude per unit time. The method involves placing the active electrode in the projection zone of the stomach on the anterior abdominal wall, which is not always possible.
- Registration of gastric biopotentials from a remote point [Rebrov VG, 1975] with the help of EGS-4M apparatus. Active electrode - on the right wrist, indifferent - on the right ankle.
- Paschelectrography is a simultaneous examination of the motor function of the stomach and intestines. The method is based on the fact that the frequency of muscle contractions is specific for different parts of the digestive tract and coincides with the frequency of the main electric rhythm [Shede H., Clifton J., 1961; Christensen J., 1971]. Selecting this frequency with the help of narrowband filters, when placing electrodes on the body surface, it is possible to follow the character of changes in the total potential of the corresponding parts of the gastrointestinal tract, including the small and large intestines.
- Radio telemetry. Intragastric pressure is determined by a capsule inserted into the stomach, including a pressure sensor and a radio transmitter. Radio signals are perceived by an antenna mounted on the patient's body, transmitted through the converter to a recording device. The curves are analyzed in the same way as for electrogastrography.
Simple, reliable informative tests for the diagnosis of vegetative insufficiency in the gastrointestinal system do not yet exist.
Genitourinary system
In this area, as yet, there are no simple informative tests of the investigation of autonomic nerves; the methods used are based on the study of the functions of the end effector organs.
Methods for determining the state of parasympathetic and sympathetic efferent pathways
- Mikruiometriya - a quantitative method, which uses special instruments - uroflowmeters - to assess the evacuation function of the urinary bladder, controlled by the parasympathetic nervous system.
- Cystometry is a quantitative method that assesses the motor and sensory functions of the bladder. Based on the relationship between intravesical pressure and the volume of the bladder, it is possible to determine the level of damage: above the spinal centers, preganglionic parasympathetic fibers, postganglionic nerves.
- Urethral pressor profilometriya - a method for assessing the state of the urethra by the constructed schedule - the pressure profile throughout its extent during urinary evacuation. Used to exclude the pathology of the lower urinary tract.
- Cystourethrography is a contrast method for revealing the dissynergy of the inner and outer sphincters.
- Ultrasound sonography is a modern non-invasive method for studying the functions of the bladder, allowing to evaluate all stages of urination and filling.
- Electromyography of the external anal sphincter is a method used to diagnose the dissection of the external sphincter of the bladder, which functions by analogy with the anal external sphincter.
- Monitoring of erections during night sleep - used for differential diagnosis of organic and psychogenic impotence. With organic lesion of parasympathetic fibers in the morning and during the night sleep, erections I are absent, while in healthy and psychogenic impotence, erections are preserved.
- The study of induced skin sympathetic potentials from the surface of the genital organs is performed to evaluate the function of sympathetic efferent nerves. When they are affected, lengthening of latency periods of responses, decrease in their amplitudes are noted.
Skin (sweating, thermoregulation)
Methods for determining the state of the efferent sympathetic pathway
- Study of induced cutaneous sympathetic potentials. The method is based on the phenomenon of GSR and consists of recording skin biopotentials in response to electrical stimulation of the median nerve. Since the sympathetic nervous system is an efferent part of GSR, the characteristics of the received response were used to analyze this part of the autonomic nervous system. Four pairs of surface electrodes (20x20x1.5 mm) are superimposed on the palms and feet. The registration is carried out with the help of an electroneuromiograph with an amplifier sensitivity of 100 μV, in the frequency range of 1.0-20.0 Hz at the epoch of analysis of 5 s. As an electrical stimulus, single irregular pulses of a rectangular shape with a duration of 0.1 s are used. The current strength is selected as standard by the appearance of the motor response of the thumb when stimulated in the area of the median nerve projection at the wrist level. Incentives are given in random order with an interval of at least 20 s after the extinction of spontaneous GSR. In response to the stimulus, 4-6 skin-galvanic responses are averaged, which are referred to as induced cutaneous sympathetic potentials. The latent periods and the I amplitude of the VKSP are determined. Informativity of this method was shown by a series of studies in patients with various forms of polyneuropathies in systemic, endocrine and autoimmune diseases. Elongation of LP and reduction of AMP of VKSP in this case was regarded as a violation of the excitation of vegetative navigating fibers, and the absence of answers as a result of gross violation of the function of the perspiration fibers. However, when analyzing VKSP, one should always take into account that the parameters of latencies and amplitudes can change not only in disorders in the peripheral, but also in the central nervous system. When interpreting VKSP data from the point of view of the level of the VNS lesion, it is necessary to take into account the results of clinical and other paraclinical methods of investigation (ENMG, VP, EEG, MRI, etc.). Advantages of the method are non-invasiveness, complete safety, quantitative evaluation of the results.
Another method is informative quantitative sudomotorny axon reflex test (QSART - quantitative sudomotor axon reflex test), in which the local sweating iontophoresis stimulated acetylcholine. The severity of sweating is recorded by a special sudorometer that transmits information in analog form to the computer. The study is conducted in a special heat insulation room at rest and under thermal loads (hot tea, etc.). The need for special premises and technical equipment for research limits the wide application of this method.
Significantly less frequently, dye samples are used to assess sweating. Some of them are described below. The suffering of the efferent part of the reflex sympathetic arch is determined by the absence of sweating on a specific part of the body. Localization is established by observing the sweating with the help of an iodine-starch Minor test or Yuzhelevsky's chromocobalt test. Sweating is achieved by various methods:
-
- Aspirin test: taking 1 g of acetylsalicylic acid with a glass of hot tea causes diffuse sweating through the use of cerebral devices; with cortical lesions, there is a monoplegic type of sweating more often - its absence or decrease.
- Warming the examinee in a drybox, heating chamber or immersion of two extremities in hot water (43 ° C) causes spinal flow reflexes through the cells of the lateral horns of the spinal cord. When the segmental parts of the spinal cord are affected, the heating procedures, as well as the aspirin test, reveal a lack or decrease in sweating in the respective areas.
- Sample with pilocarpine: subcutaneous administration of 1 ml of a 1% solution of pilocarpine, acting on the end-capillary devices, causes normal sweating in a specific area of the body. Absence or decrease in sweating with this sample is observed in the absence or lesion of sweat glands.
- Examination of an axon reflex: stimulation with a Faradic current, intradermal injection of acetylcholine (5-10 mg) or electrophoresis of acetylcholine after 5 minutes causes local piloerection and sweating. The absence of piloerectomy, the decrease or absence of sweating indicate a lesion of sympathetic ganglia or postganglionic neurons.
- Investigation of surface skin temperature with the help of thermal imagers: the intensity of infrared radiation is recorded, which is the essence of the thermograms obtained. The effects of an isotherm are used to quantify the value of infrared radiation. The temperature is recorded in degrees. Interpretation of thermograms is based on the presence of thermal asymmetry, as well as the magnitude of the longitudinal terminal gradient reflecting the temperature difference between the distal and proximal areas of the skin. The study of thermograms and the intensity of skin temperature showed that the upper half of the body is warmer than the lower one, the right and left extremities are characterized by a symmetrical image, the proximal parts of the extremities are warmer than the distal ones, and the difference is insignificant and gradual. In patients with cerebral vegetative disorders, the distribution of skin temperature by thermographic parameters is represented by the following types:
- bilateral "thermoamputation" at the level of the lower third of the forearm with hypothermia of hands and feet, with a sharp temperature drop of 2-4 ° C;
- hyperthermia of the hands and feet, more common in patients with hypothalamic syndrome;
- different types of asymmetries:
- one-sided "thermoamputation" of the brush;
- asymmetry "thermoamputation" of hands and feet.
With the defeat of segmental parts of the autonomic nervous system, various types of asymmetries are observed.
Pupil
It is known that the sympathetic and parasympathetic systems innervate the muscles that dilate and contract the pupil. Non-neuropharmacological research makes it possible to distinguish pre- and postganglionic lesions of vegetative nerves innervating the muscles of the iris. The analysis makes it possible to differentiate the occurrence of ptosis and miosis due to damage to the sympathetic fibers of the pupillary dilating muscle from Horner's syndrome, which is based on the more proximal damage to the sympathetic pathways that lead to this muscle, as well as the Ady's syndrome (tonic dilatation of the pupils) with damage to postganglionic parasympathetic fibers innervating the muscle, narrowing the pupil, and also from mydriasis, which arose when the preganglionic fibers were damaged.
The neuropharmacological method of analysis is based on the phenomenon of denervation hypersensitivity of postganglionic sympathetic and parasympathetic fibers. It has been shown that if, in miosis or ptosis, there is denervational hypersensitivity of the narrowed pupil, then the lesion is localized not in the preganglionic sympathetic fiber, but in the postganglionic on the base of the skull or along the internal carotid artery. If there is a denervation hypersensitivity of the dilated pupil with mydriasis, it is also unlikely that the preganglionic fibers in the brainstem, the cavernous sinus, or the cervical spinal cord are damaged. This is typical for damage to sympathetic postganglionic fibers or in the ciliary node, or in the outer layers of the eye.
When studying pupils and carrying out neuropharmacological tests, there are several rules:
- in each eye instilled 1 drop of the drug at intervals of 2 minutes;
- as the test is conducted to identify a defect, it may be necessary to triple instillation at 10-minute intervals, i.e. 6 drops per eye;
- in patients with a one-sided violation of the size of the pupil, both pupils should be examined;
- denervation hypersensitivity is considered to be detected if the dilated pupil is contracted and the other does not respond. If there is no answer, then the concentration of the drug can be increased provided that both eyes are examined. Denervation hypersensitivity of the dilated pupil can be excluded only if the normal pupil begins to contract in the absence of a stronger contraction of the dilated pupil.
In the bilateral pathology of pupils, it is impossible to compare, only one eye needs to be examined, and the other will serve as a control.
Tests for sympathetic denervation hypersensitivity in miosis
- Introduction 0.1% solution of adrenaline: the normal pupil does not expand in response to instillation of epinephrine. With denervation hypersensitivity, adrenaline causes mydriasis. Maximum hypersensitivity occurs when the postganglionic sympathetic pathway is damaged. The pupil dilates by more than 2 mm. Adrenaline does not cause a significant change in the size of the pupil when the preganglionic sympathetic fibers are damaged (especially the "first neuron"), that is, with the complete Horner syndrome this sample is negative.
- Test with 4% cocaine solution: cocaine is rarely used in isolation, because it does not allow you to specify the place of damage to the sympathetic nerve, it is often used in combination with an adrenaline test. Combined test method: 2 drops of 4% cocaine solution are injected, if necessary, this is repeated three times. A distinct mydriasis with miosis indicates damage to the pregan-glionic sympathetic fiber. If there is no reaction, then after 30 minutes a 0.1% solution of epinephrine is instilled: a small dilatation of the pupil may indicate a possible damage to the preganglionic fiber, its "second neuron"; The distinct dilatation of the pupil is a diagnostic sign of damage to the postganglionic sympathetic fiber.
Test for parasympathetic denervation hypersensitivity in mydriasis
2.5% mecholyl drops are used. Enter 1 drop of solution into each eye with repeated instillation in 5 minutes. Tonic dilated pupil reacts to mecholil with expressed miosis. There is no reaction in the intact pupil. This test is informative in the syndrome of Adi.
Internal ophthalmoplegia: the identification of its causes does not need to carry out pharmacological tests, neurological topical analysis is needed.
In addition to pharmacological samples, there are others.
- Pupil cycle time. Using a slit lamp, a narrow strip of light is fed through the edge of the pupil. In response, rhythmic contractions and narrowing of the pupil are observed. The time of one such cycle (narrowing-expansion) in healthy people is 946 ± 120 ms. The increase in the time of the pupillary cycle indicates a parasympathetic insufficiency.
- Polaroid photographing of the pupil with an electronic flash is a method that makes it possible to determine the size of the pupil in the dark. The determination of the size of the pupil adapted to the darkness with respect to the external diameter of the iris makes it possible to assess the state of sympathetic innervation. Insufficient dilatation of the pupil indicates sympathetic failure. The method is sensitive to minimal changes in the sympathetic function.
- Infrared television papillomometry is a quantitative method that allows to determine the exact dimensions of the pupil at rest, in response to light and in the dark, which provides extensive information for evaluating the autonomic innervation of the pupil.
- Heterochromia of the iris: the sympathetic nervous system influences the formation of melanin and determines the color of the iris. Disturbance of pigmentation of one iris testifies to damage of sympathetic fibers even in the early childhood. Depigmentation in adults is extremely rare. The cause of heterochromia in adults may be a local disease or the result of a congenital isolated anomaly. Depigmentation can be observed with other symptoms of sympathetic innervation damage in Horner's syndrome (more often - congenital).
What do need to examine?
Last reviewed: 26.06.2018
