
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Herpetic keratouveitis and glaucoma
Medical expert of the article
Last reviewed: 04.07.2025
Herpes simplex virus (HSV) infection of the eye manifests itself as recurrent unilateral blepharoconjunctivitis, epithelial and stromal keratitis, and uveitis. Eye involvement can also be seen in primary herpes zoster (chickenpox) infection, but is more common in herpes zoster ophthalmicus, a reactivation of the herpes zoster virus in adults with lesions of the ophthalmic branch of the 5th cranial nerve.
Uveitis caused by HSV and herpes zoster virus accounts for about 5% of all uveitis in adults, and usually develops against the background of herpetic keratitis. A characteristic feature of recurrent herpetic uveitis is an increase in intraocular pressure, which can lead to the development of secondary glaucoma.
Epidemiology
Approximately 0.15% of the US population has a history of ocular manifestations of HSV infection. Ocular involvement occurs in two-thirds of herpes zoster ophthalmicus infections. Stromal keratitis and uveitis are the most visually impaired of all forms of recurrent herpes ocular disease. Stromal keratitis and uveitis occur in less than 10% of patients with primary herpes simplex ocular infection. Uveitis and ocular hypertension in patients with herpes zoster ophthalmicus may be associated with epithelial or stromal keratitis. The incidence of increased intraocular pressure in patients with herpes uveitis is 28-40%. The incidence of secondary glaucoma in patients with herpes simplex or herpes zoster uveitis is 10-16%.
Causes of herpetic keratouveitis
Whether the development of uveitis associated with herpes simplex keratitis is secondary to corneal damage or is associated with viral invasion of the anterior choroid is currently unknown. Increased intraocular pressure in herpes simplex and herpes zoster uveitis occurs as a result of impaired outflow of intraocular fluid due to trabeculitis - inflammation of the trabecular network. In uveitis caused by herpes zoster, ischemia associated with occlusive vasculitis develops, which can also lead to an increase in intraocular pressure. In herpetic uveitis, herpes simplex was isolated from the fluid of the anterior chamber, the presence of which probably correlates with the development of ocular hypertension. An increase in intraocular pressure in herpetic uveitis can also be associated with long-term use of glucocorticoids.
Symptoms of herpetic keratouveitis
Patients with herpetic uveitis typically present with redness in one eye, pain, photophobia, and decreased visual acuity. There is often a history of recurrent keratitis. Patients with herpes zoster uveitis are usually older with a history of herpes zoster ophthalmicus. Rarely, HSV affects the eye bilaterally, while herpes zoster affects the eye only unilaterally.
 [ 10 ], [ 11 ], [ 12 ], [ 13 ]
[ 10 ], [ 11 ], [ 12 ], [ 13 ]
Course of the disease
Like other manifestations of herpetic eye lesions, herpetic uveitis is recurrent and may occur against the background of recurrent keratitis. During exacerbation of intraocular inflammation, an increase in intraocular pressure is usually observed, which may normalize or remain elevated as uveitis resolves. In approximately 12% of cases, persistent increase in intraocular pressure develops, requiring antiglaucoma therapy or surgery to improve filtration.
Ophthalmological examination
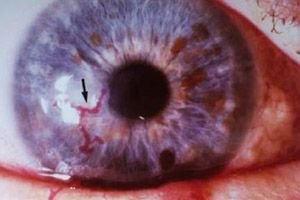
On external examination, signs of iridocyclitis (herpes zoster skin lesions), conjunctival and ciliary injection are revealed. Corneal sensitivity in the affected eye is often decreased. On examination of the cornea in patients with herpetic keratouveitis, changes are revealed that indicate previous damage to the corneal epithelium or stroma (dendritic epithelial foci, dendritic opacities, active disciform or necrotic stromal keratitis, neovascularization or scarring). In two forms of herpetic uveitis, diffuse nongranulomatous stellate or pigmented granulomatous precipitates on the cornea can be detected. In severe herpetic uveitis, posterior synechiae and closure of the anterior chamber angle can be detected. In uveitis caused by both the herpes simplex virus and herpes zoster, characteristic atrophy of the iris develops. In HSV lesions, atrophy occurs in the central part of the iris closer to the pupil, often has a spotty appearance, and in herpes zoster lesions, iris atrophy has a segmental character and is localized closer to the periphery. It is believed that in herpes zoster lesions, the cause of iris atrophy is occlusive vasculitis in the stroma.
 [ 14 ]
[ 14 ]
Laboratory research
The diagnosis of herpetic uveitis is made on the basis of clinical data and usually does not require laboratory testing. In the absence of antibodies to HSV and varicella zoster virus, the diagnosis of herpetic uveitis is excluded. Detection of viral DNA in the intraocular fluid by polymerase chain reaction confirms the diagnosis of herpetic uveitis, but does not allow it to be made.
Treatment of herpetic keratouveitis
In uveitis associated with HSV or herpes zoster, topical glucocorticoids are prescribed. In case of pain syndrome associated with ciliary spasm, the use of cycloplegic drugs may be required. To reduce the risk of recurrence of epithelial keratitis, in addition to topical glucocorticoids, an antiviral drug should be prescribed. It has been shown that oral acyclovir reduces the incidence and severity of dendritic keratitis, stromal keratitis and uveitis in patients with herpes zoster ophthalmicus. If intraocular pressure increases, antiglaucoma therapy should be administered. Sometimes, surgery to improve filtration may be required. Argon laser trabeculoplasty is considered ineffective in herpetic uveitis.

