
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Hemosorption in the treatment of bronchial asthma
Medical expert of the article
Last reviewed: 04.07.2025
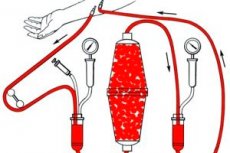
Hemosorption is considered as a method of detoxification (when blood passes through a hemosorbent, toxins are removed) and immunocorrection (the function of lymphocytes and phagocytes is activated, the number of receptors for cortisol on the surface of lymphocyte membranes increases).
Hemosorption has proven effective in atopic bronchial asthma, including polyvalent allergy and corticosteroid-dependent corticosteroid-resistant bronchial asthma. After hemosorption, the effectiveness of drug therapy increases.
Hemosorption is often effective in people with an unidentified allergen. After hemosorption, it is possible to identify the "culprit" of the allergy (i.e. the cause of bronchial asthma). Hemosorption is contraindicated in case of exacerbation of infection in the bronchopulmonary system.
Extracorporeal immunosorption
Extracorporeal immunosorption is a method based on the removal of specific IgE reagins from the bloodstream of patients by passing blood through a sorbent on which the allergen of house dust and timothy grass pollen are immobilized. Specific IgE react with allergens and precipitate on the sorbent. The method is indicated for severe cases of atopic bronchial asthma, low efficiency of specific immunotherapy and traditional treatment of the disease. Extracorporeal immunosorption also helps to increase the number of beta-adrenoreceptors in the bronchi.
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ]
Monoclonal anti-IgE immunoadsorption
Monoclonal anti-IgE immunosorption involves removing reagins from the patient's body by passing blood through a sorbent containing monoclonal antibodies to IgE. This method can be used in patients with bronchial asthma, sensitized to a large number of allergens, for the same indications as extracorporeal immunosorption.
Plasmapheresis
Plasmapheresis is the removal of the patient's plasma (reagins are removed along with it) and its replacement with a plasma substitute. The method is used in severe, treatment-resistant forms of bronchial asthma.
The mechanism of therapeutic action of plasmapheresis:
- detoxification;
- immunocorrective effect;
- correction of blood rheological properties and improvement of microcirculation in the lungs;
- increased activity of glucocorticoid receptors in the bronchi;
- reduction of the inflammatory process in the bronchi (primarily the eosinophilic component of inflammation);
- increasing blood oxygen saturation;
- increasing the sensitivity of bronchopulmonary system cells to therapeutic measures.
The volume of plasma removed is 30-40% of the volume of plasma circulating in the bloodstream. The volume of plasma substitute exceeds the volume of plasma removed by 30%. 2-5 plasmapheresis procedures are performed at intervals of 2-3 days.
The plasmapheresis method can be used for all types of bronchial asthma, but it is most effective for the atonic form of the disease. Plasmapheresis is also highly effective for asthmatic status in combination with pulse therapy with prednisolone.
Contraindications to plasmapheresis:
- absolute - epilepsy, tendency to thrombosis;
- relative - age over 60 years, circulatory failure II B and III stage; anemia; hypotension; cardiac arrhythmia.
Lymphocytapheresis, thrombocytapheresis and enterosorption
Lymphocytapheresis - removal of cytotoxic lymphocytes from the blood by gravity. Indications are the same as for plasmapheresis.
Thrombocytapheresis is the removal of platelets from the blood. Platelets play an important pathogenetic role in the development of bronchial asthma. Patients with bronchial asthma have increased platelet aggregation and microcirculation disorders. Platelets, along with mast cells, alveolar macrophages, and eosinophils, produce platelet-activating factor (PAF), which contributes to the development of bronchospasm, cellular infiltration, and edema of the bronchial mucosa.
Thrombocytapheresis is effective in 90% of patients with atopic bronchial asthma. The therapeutic effect of thrombocytapheresis is due to the normalization of the aggregation capacity of platelets, a decrease in their release of PAF, which is involved in the development of inflammation in bronchial asthma.
Enterosorption is most widely used in the treatment of atopic bronchial asthma caused by drug and food allergies.

