
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Examination of the esophagus
Medical expert of the article
Last reviewed: 05.07.2025
The study of complaints is of the greatest importance in the clinical diagnosis of esophageal diseases.
Dysphagia is difficulty swallowing, the passage of food through the esophagus. Pharyngeal dysphagia is difficulty swallowing a bolus of food (sometimes with coughing), it is usually caused by neuromuscular disorders. Esophageal dysphagia is characterized by the progression of the process over weeks and months, a violation of the passage of first solid and then liquid food. The sensation of a lump in the throat or behind the breastbone, not associated with swallowing food (pseudodysphagia), is observed with gallstones, heart disease, but most often with hysteria.
Painful swallowing and passage of food through the esophagus is a serious sign of various esophageal diseases. Belching of food masses is characterized by the involuntary appearance of gastric contents in the mouth. It is often accompanied by aspiration of food masses - their entry into the respiratory tract (choking with the appearance of a cough). Most often, aspiration of food masses with the development of pneumonia occurs in patients with alcoholism.
Burning and severe pain behind the breastbone, indistinguishable from the pain of angina pectoris and myocardial infarction, occur when food is thrown from the stomach into the esophagus ( reflux ).
Physical research methods
Examination of the esophagus itself using physical methods is difficult to access. However, if the above complaints are present, a general examination and examination of other organs is performed.
Examination reveals decreased nutrition and even general exhaustion associated with impaired food intake in the stomach due to cancer and achalasia of the esophagus. Signs of a systemic disease, such as systemic scleroderma, may be detected in the form of characteristic facial amimia, skin thickening, etc.
With long-term narrowing of the esophagus, there is a significant expansion of the part located above, sometimes with displacement of the adjacent part of the lungs, a decrease in their vital capacity and the development of respiratory failure of the restrictive type.
An objective examination of a patient suffering from one or another disorder of the esophagus is divided into general and local.
A general examination, in addition to the generally accepted methods prescribed by the relevant specialist (gastroenterologist, surgeon, ENT doctor, etc.) includes an examination of the patient, during which attention is paid to his behavior, reaction to questions asked, complexion, nutritional status, visible mucous membranes, skin turgor, its color, dryness or moisture, body temperature. Extreme anxiety and a corresponding grimace on the face, a forced position of the head or body bent forward indicate a pain syndrome, which can be caused by the presence of foreign bodies, food impaction, a diverticulum filled with food, mediastinal emphysema, periesophagitis, etc. In such cases, the patient is usually tense, tries not to make unnecessary movements of the head or body, takes a position in which chest (esophagus) pain is minimized.
A relaxed and passive state of the patient indicates traumatic (interstitial injury, burn) or septic (periesophagitis or a perforating foreign body complicated by mediastinitis) shock, internal bleeding, general intoxication in the case of poisoning with an aggressive liquid.
The patient's facial expression reflects his mental state and partly the nature of the disease. Painful sensations arising in severe pathological conditions of the esophagus, such as chemical burns, perforations, secondary esophagomediastinitis, cause fear in the patient, a feeling of hopelessness of his situation and extreme anxiety. Sometimes in septicemia and severe injuries - a delirious state.
Mental disorders are usually observed in acute diseases and lesions of the esophagus, while in chronic stenosis, patients develop a state of depression, pessimism, and indifference.
When examining a patient, the color of the skin of the face is assessed: pallor - in case of traumatic shock, pallor with a yellowish tint - in case of esophageal (stomach) cancer and hypochromic anemia, redness of the face - in case of acute vulgar esophagitis, cyanosis - in case of volumetric processes in the esophagus and mediastinal emphysema (compression of the venous system, respiratory failure).
When examining the neck, attention is paid to the presence of soft tissue edema, which may occur with inflammation of the periesophageal tissue (differentiate from Quincke's edema - acute angioedema of the face, mainly the lips and eyelids, neck, limbs and external genitalia, often also affecting the tongue, mucous membrane of the cheeks, epiglottis, less often the lower parts of the larynx), to the skin veins, the increased pattern of which may indicate the presence of cervical lymphadenopathy, a tumor or diverticulum of the esophagus. Increased venous pattern on the skin of the abdomen indicates the development of cavocaval collaterals due to compression of the vena cava (mediastinal tumor) or the presence of varicose veins of the esophagus with difficulty of venous outflow in the portal vein system of the liver (liver cirrhosis). In the latter case, esophageal bleeding is often observed, and if the blood immediately gets into the oral cavity, it is red, if first into the stomach cavity, where it reacts with hydrochloric acid, and then regurgitates, it becomes dark red, almost black. Consequently, the dark color of blood in vomit may indicate not only gastric, but also esophageal bleeding.
Local examination of the esophagus includes indirect and direct methods. Indirect methods include palpation, percussion and auscultation; direct methods include radiography, esophagoscopy and some others. Only the cervical esophagus is accessible to palpation, but in this case there are massive tissues and a number of organs on the way to the esophagus that prevent this manipulation. The lateral surfaces of the neck are palpated by inserting fingers into the space between the lateral surface of the larynx and the anterior edge of the sternocleidomastoid muscle. In this area, painful points and foci, enlarged lymph nodes, crepitation of air in emphysema of the cervical mediastinum, a tumor, sound phenomena during emptying of the diverticulum, etc. can be detected. Percussion can establish a change in percussion tone, which in emphysema or stenosis of the esophagus acquires a tympanic tint, in case of a tumor it does not change or becomes duller. Auscultation provides an idea of the nature of the passage of liquid and semi-liquid substances through the esophagus, and so-called swallowing noises are heard.
Additional research methods
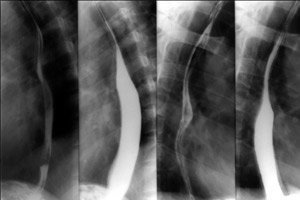
X-ray examination. It is very demonstrative and often has a decisive significance for diagnosis. In this case, the patient swallows a contrast mixture, and as it passes through the esophagus, the mucous membrane, motor activity, changes in the contour of the esophagus can be examined: expansion, retraction, irregularities (inflammatory changes, tumors).
X-ray examination of the esophagus, along with fibroesophagoscopy, is the most common method used in diagnosing diseases of this organ. There are a large number of techniques that make up this method, which pursue various diagnostic goals, such as teleradioscopy and teleradiography, which prevent deformation of foreign bodies, or orthodiagraphy, which is used to take measurements between two radio-contrast markers for projection localization of esophageal deformations, its expansions, or identification of foreign bodies. Tomography, including CT, allows determining the extent of the pathological process; stereoradiography forms a three-dimensional image and determines the localization of the pathological process in space. Roentgenokymography allows recording peristaltic movements of the esophagus and identifying their disorders. Finally, CT and MRI allow obtaining comprehensive tomographic information on the localization of the pathological process and the nature of organic changes in its walls and surrounding tissues.
The esophagus is not radiopaque. Sometimes, with very "soft" radiation, it is possible to visualize it as a weak shadow with contoured edges. The esophagus becomes visible when air accumulates in it or in the space surrounding it, which can be observed with aerophagia, paretic dilation of the esophagus, emphysema of the periesophageal space. The origin of the latter can be due to perforation of the esophageal wall, gas infection of the mediastinum, etc.
For good visualization of the esophagus, artificial contrast methods are used (introduction of air through a probe or the use of sodium bicarbonate, which, when in contact with hydrochloric acid of the gastric juice, releases carbon dioxide, which enters the esophagus during belching). However, barium sulfate is most often used as a contrast agent. Sometimes, iodolipol is used. The use of radiocontrast agents of different aggregate states pursues different goals, primarily such as determining the filling of the esophagus, its shape, the state of the lumen, patency and evacuation function.
Special methods of regional lymph node examination are of great importance in diagnosing esophageal diseases. Thus, in certain diseases, most often oncological, of the pharynx and upper esophagus, as well as in purulent and other inflammatory processes in this area, the lymph nodes of the neck are involved in the pathological process, which, according to N.L. Petrov (1998), respond with a lymphadenopathic reaction to more than 50 described nosological forms, while the nature of lymphadenopathy can be differentiated by physical examination only in 70% of cases. According to N.V. Zabolotskaya (1996), in patients over 40 years of age, the proportion of malignant neoplasms among all possible lymphadenopathies is 60%.
Endoscopy. This is the most sensitive method of studying the esophagus. Material is taken from the changed areas of the mucous membrane for histological and bacteriological studies. Changes in the esophagus associated with reflux can be studied visually.
An important indication for endoscopy is bleeding from the upper gastrointestinal tract, which allows detection of varicose veins, esophageal cancer, etc.
Perfusion of the esophageal mucosa is performed by inserting a special probe and alternately irrigating the lower third of the esophagus with neutral or acidic (low pH) liquid. Unpleasant sensations that the patient notes during irrigation with acidic liquid indicate the presence of esophageal pathology.
Esophageal manometry. This study is performed to assess the contractile function of the esophageal muscles. Special sensors are inserted using a catheter and placed at different levels of the esophagus. The patient is then asked to swallow liquid. At the level of the lower esophageal sphincter, pressure from 20 to 40 mm Hg normally develops. The pressure may be higher, and the ability of the sphincter to relax is reduced in achalasia of the esophagus.
Measuring the pH of the contents of the lower esophagus allows the diagnosis of reflux, in which case the pH of the contents decreases.


 [
[