
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
How does phosphorus affect human health?
Medical expert of the article
Last reviewed: 03.07.2025

Phosphorus is an essential mineral that is present in every cell of the body to perform their normal functions. Most of the phosphorus in the body is found as phosphate (PO 4). About 85% of the body's phosphorus is found in the bones. How does phosphorus affect human health?
Phosphorus and its effects on the human body
Like calcium, phosphorus is the most abundant mineral in the body. These two important nutrients work closely together to maintain strong bones and teeth. About 85% of the body's phosphorus is found in bones and teeth, but it is also present in cells and tissues throughout the body.
Phosphorus helps filter waste in the kidneys and plays an important role in how the body uses energy. It also helps reduce muscle soreness after a hard workout. Phosphorus is needed for the growth, repair, and regeneration of all tissues and cells, as well as the production of the genetic building blocks, DNA and RNA. Phosphorus is also needed to help balance and utilize other vitamins and minerals, including vitamin D, iodine, magnesium, and zinc.
The use of phosphorus for treatment
- Phosphates (phosphorus) are used clinically to treat the following diseases
- Hypophosphatemia, low levels of phosphorus in the body
- Hypercalcemia, high levels of calcium in the blood
- Calcium is the basis of kidney stones
These ailments require mandatory examination by a doctor.
Phosphates are used in the same way in enemas as a laxative. Most people get plenty of phosphorus in their diet. Athletes sometimes use phosphate supplements before competitions or hard workouts to help reduce muscle soreness and fatigue, although it is unclear how much this helps or improves performance.
Phosphorus in the diet
Most people get plenty of phosphorus in their diet. Mineral supplements of phosphorus are found in milk, grains, and protein-rich foods. Certain medical conditions, such as diabetes, starvation, and alcoholism, can cause phosphorus levels in the body to drop.
The same goes for conditions that prevent people from absorbing nutrients, such as Crohn's disease and celiac disease. Certain medications can cause low phosphorus levels, including some antacids and diuretics (water pills).
Phosphorus absorption
Phosphorus is absorbed more efficiently than calcium. Almost 70 percent of phosphorus is absorbed from the intestine, although this rate depends on calcium and vitamin D levels and the activity of parathyroid hormone (PTH), which regulates phosphorus and calcium metabolism. Most phosphorus is deposited in bones, a little goes to teeth, and the rest is contained in cells and tissues. A lot of phosphorus is found in red blood cells. Plasma contains about 3.5 mg of phosphorus. (3.5 mg of phosphorus per 100 ml of plasma), and the total amount of phosphorus in the blood is 30-40 mg.
In the body, the level of this mineral is regulated by the kidneys, which are also influenced by PTH. Phosphorus absorption can be reduced by antacids, iron, aluminum or magnesium, which can form insoluble phosphates that are excreted in the feces. Caffeine causes an increase in phosphorus excretion by the kidneys.
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ]
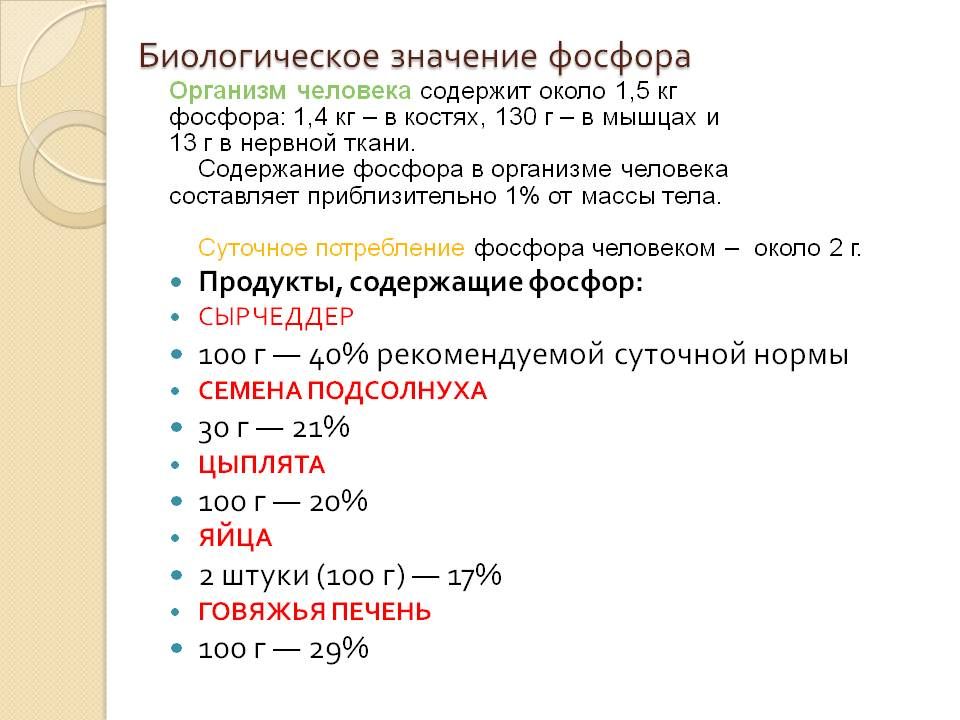
Food sources of phosphorus

Protein-rich foods such as meat, poultry, fish, eggs, dairy products, nuts, and legumes are good sources of phosphorus. Other sources include whole grains, potatoes, dried fruits, garlic, and carbonated beverages.
Since phosphorus is a component of all cells, it is easy to find foods, especially those of animal origin, that can provide phosphorus. Most protein foods are high in phosphorus. Meat, fish, chicken, turkey, milk, cheese, and eggs contain significant amounts. Most red meat and poultry contain much more phosphorus than calcium, 10 to 20 times more, while fish typically contains about 2 to 3 times more phosphorus than calcium. Dairy products contain a more balanced calcium-phosphorus ratio.
Seeds and nuts also contain high levels of phosphorus (though they have much less calcium), as do whole grains, brewer's yeast, wheat germ, and bran. Most fruits and vegetables contain some phosphorus and can help balance the phosphorus-to-calcium ratio in a healthy diet.
Symptoms of Phosphorus Deficiency
Symptoms of phosphorus deficiency include loss of appetite, restlessness, bone pain, brittle bones, stiff joints, fatigue, shortness of breath, irritability, numbness, weakness, and weight changes. In children, this includes decreased growth and deterioration of bones and teeth.
Too much phosphorus in the body is actually more of a concern than too little. Too much phosphorus is usually caused by kidney disease or by people consuming too much dietary phosphorus and not enough dietary calcium.
Some studies show that higher phosphorus intake is associated with an increased risk of cardiovascular disease. As phosphorus intake increases, the need for calcium increases. A delicate balance between calcium and phosphorus is essential for proper bone density and the prevention of osteoporosis.
Available forms of phosphorus
Elemental phosphorus is a white or yellow waxy substance that burns when exposed to air. Phosphorus is highly toxic and is used in medicine only as a homeopathic treatment. For this reason, you should only take phosphorus products under the guidance of a qualified professional. Instead, health care professionals may use one or more of the following inorganic phosphates, which are nontoxic at typical normal doses:
- Dibasic potassium phosphate
- Potassium phosphate monobasic
- Sodium phosphate dibasic
- Monosodium phosphate
- Tribasic sodium phosphate
- Phosphatidylcholine
- Phosphatidylserine
Pediatric Doses of Phosphorus
| Age | mg/day |
| For babies 0 - 6 months | 100 |
| For children 7 - 12 months | 175 |
| For children 1 - 3 years old | 460 |
| For children 4 - 8 years old | 500 |
| For children 9 - 18 years old | 1250 |
Phosphorus Doses for Adults
| Adults 19 years and older | 700 mg |
| Pregnant and lactating women under 18 years of age | 1250 mg |
| Pregnant and lactating women 19 years and older | 700 mg |
Phosphorus for Seniors (51 and Up)
There is currently no evidence that phosphorus doses for older adults are different from those for younger adults (700 mg/day). Although some multivitamin/mineral supplements contain more than 15% of the current daily phosphorus intake, a varied diet can easily provide adequate phosphorus for most older adults.
Nutritional interactions of phosphorus with other elements
Fructose
A US study of 11 adult men found that a high-fructose diet (20% of total calories) led to an enlarged bladder, loss of phosphorus, and a negative phosphorus balance (ie, daily phosphorus loss was greater than the daily intake). This effect was more pronounced when the men's diets contained low levels of magnesium.
A potential mechanism for this effect is the absence of feedback inhibition of fructose conversion in the liver. In other words, fructose-1-phosphate accumulates in cells, but this compound does not inhibit the enzyme that phosphorylates fructose, which consumes large amounts of phosphate. This phenomenon is known as phosphate uptake.
The findings of this study are important because fructose consumption in the United States has increased rapidly since the introduction of high-fructose corn syrup in 1970, while magnesium consumption has declined over the past century.
Calcium and Vitamin D
Phosphorus is readily absorbed in the small intestine, and any excess phosphorus is excreted via the kidneys. The regulation of blood calcium and phosphorus are interrelated through the action of parathyroid hormone (PTH) and vitamin D. A slight decrease in blood calcium (for example, in the case of insufficient calcium intake) is sensed by the parathyroid glands, resulting in increased secretion of parathyroid hormone (PTH).
This hormone stimulates the conversion of vitamin D into its active form (calcitriol) in the kidneys.
Increased levels of calcitriol, in turn, lead to increased intestinal absorption of trace elements such as calcium and phosphorus. Both substances - parathyroid hormone - PTH - and vitamin D - stimulate bone resorption, resulting in increased levels of bone tissue (calcium and phosphate) in the blood. Although PTH results in stimulation and decreased excretion of calcium, this leads to increased excretion of phosphorus in the urine.
Increasing urinary phosphorus excretion is beneficial, resulting in blood calcium levels falling to normal, because high blood phosphate levels inhibit the conversion of vitamin D to its active form in the kidneys.
How bad is high phosphorus intake for bone health?
Some researchers are concerned about the increase in phosphate in food, which can be attributed to phosphoric acid in soft drinks and phosphate additives in some foods. Because phosphorus is not as tightly regulated by the body as calcium, serum phosphate levels may rise slightly with high phosphorus intake, especially after meals.
High blood phosphate levels reduce the formation of the active form of vitamin D (calcitriol) in the kidneys, lower blood calcium levels, and may increase PTH release from the parathyroid glands. However, high phosphorus levels may also reduce urinary calcium excretion. Elevated PTH levels may have adverse effects on bone mineral content, but this effect has only been observed in people on high-phosphorus, low-calcium diets.
In addition, similarly elevated PTH levels have been reported in diets low in calcium but low in phosphorus. In a recent study of young women, researchers found no adverse effects of a phosphorus-rich diet (3,000 mg/day). It did not negatively affect bone, hormone levels, or biochemical markers of bone resorption, even when dietary calcium intake was maintained at nearly 2,000 mg/day.
There is currently no convincing evidence that dietary phosphorus intake can negatively affect bone mineral density. However, replacing phosphate-containing soft drinks and snacks with milk and other calcium-rich foods does pose a serious risk to bone health.
Possible interactions of phosphorus
If you are currently being treated with any of the following medications, you should not use phosphorus preparations without talking to your doctor.
Alcohol
Alcohol can leach phosphorus from bones and cause low levels in the body.
Antacids
Antacids containing aluminum, calcium, or magnesium (such as Mylanta, Amphojel, Maalox, Riopan, and Alternagel) can bind phosphates in the intestines. If used long-term, these antacids can lead to low phosphate levels (hypophosphatemia).
Anticonvulsants
Some anticonvulsant drugs (including phenobarbital and carbamazepine or Tegretol) can decrease phosphorus levels and increase levels of alkaline phosphatase, an enzyme that helps remove phosphate from the body.
Bile acid
Bile acid preparations lower cholesterol. They may reduce the oral absorption of phosphate from food or supplements. Oral phosphate supplements should be taken at least 1 hour before or 4 hours after these preparations. Bile acid preparations include:
- Cholestyramine (Questran)
- Colestipol (Colestid)
- Corticosteroids
Corticosteroids, including prednisolone or methylprednisolone (Medrol), increase the level of phosphorus in the urine.
Insulin
High doses of insulin can lower phosphorus levels in people with diabetic ketoacidosis (a condition caused by severe insulin deficiency).
Potassium or potassium-sparing diuretics
Using phosphorus supplements with potassium or potassium-sparing diuretics can cause too much potassium in the blood (hyperkalemia). Hyperkalemia can become a serious problem, resulting in life-threatening abnormal heart rhythms (arrhythmias). Potassium and potassium-sparing diuretics include:
- Spironolactone (Aldactone)
- Triamterene (Dyrenium)
- ACE inhibitors (blood pressure medication)
These are drugs called angiotensin-converting enzyme (ACE) inhibitors used to treat high blood pressure, and they can lower phosphorus levels. They include:
- Benazepril (Lotensin)
- Captopril (Capoten)
- Enalapril (Vasotec)
- Fosinopril (monopril)
- Lisinopril (Zestril, Prinivil)
- Quinapril (Accupril)
- Ramipril (Altace)
Other medications
Other medications can also lower phosphorus levels. These include cyclosporine (used to suppress the immune system), cardiac glycosides (digoxin or Lanoxin), heparins (blood thinners), and nonsteroidal anti-inflammatory drugs (such as ibuprofen or Advil).
Salt substitutes that also contain high levels of potassium and phosphorus may result in decreased levels when used long-term.
Precautionary measures
Because of possible side effects and interactions with prescription and over-the-counter medications, you should only take phosphorus supplements under the supervision of a knowledgeable healthcare professional.
Too much phosphate can be toxic to the body. It can lead to diarrhea and calcification of organs and soft tissues, and can interfere with the body's ability to use iron, calcium, magnesium, and zinc. Athletes and other physically active people can take phosphate supplements, but should do so only occasionally and under the guidance and direction of a physician.
Nutritionists recommend a balance of calcium and phosphorus in the diet. The typical Western diet, however, contains about 2 to 4 times more phosphorus than calcium. Meat and poultry contain 10 to 20 times more phosphorus than calcium, and carbonated drinks such as cola contain 500 mg of phosphorus per serving. When there is more phosphorus than calcium in the body, the body will use the calcium that is stored in the bones.
This can cause osteoporosis (brittle bones) and also lead to gum and tooth disease. A balance of dietary calcium and phosphorus can reduce the risk of osteoporosis.

