
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Intestinal dysbacteriosis in newborns: signs, tests
Medical expert of the article
Last reviewed: 04.07.2025
Dysbacteriosis in a newborn is a common problem in children, although it is not often diagnosed and measures are taken in time. It can often be biased under the guise of other pathologies that cause problems in the child. The causes and risk factors of this pathology are varied, but the etiological principle is not so important for treatment. Therefore, if your baby has colic, stool disorders, he screams and worries - this may be one of the signs of dysbacteriosis.
Epidemiology
Statistics show that absolutely every child at a certain stage of their life faces the problem of dysbacteriosis. In the neonatal period, this happens to less than 10% of children. Speaking about the structure of the causes, the main one is considered to be the use of antibiotics in children of the first month of life, given the lability of the intestinal flora. Later, about 78% of children have functional diseases of the digestive organs at a young age. This proves the role of rational use of antibiotics and the prevalence of the problem today.
Causes infant dysbiosis.
When talking about the causes of dysbacteriosis, we must first understand the features of the functioning of the gastrointestinal tract in a child after birth, as well as the features of the microflora under normal conditions. A child is born with a sterile intestine, and only after some time does it begin to be populated by various microorganisms. This is explained by the fact that in utero the child was fed through the placenta and all the necessary nutrients passed through the vessels. The intestines had no contact with food, so there is an absolutely inert environment in terms of microflora. Immediately after birth, the baby is placed on the mother's stomach, and then on the chest - and from this moment on, contact with the skin and the bacteria that are there begins. These bacteria are a normal environment for the mother, and therefore for her child as well. And after the first day after birth, the first sterile phase ends. Already on the second day, the child's intestines begin to be actively populated by normal microflora. It is during this period that the child is vulnerable to the development of dysbacteriosis, when the flora does not have the composition it should have.
Bacterial colonization of the small and large intestines of a newborn occurs due to microorganisms that are on the mother's skin and mucous membranes, as well as due to the external environment. Therefore, at first, the child is dominated by coccal flora - streptococci, staphylococci, enterococci. A few days after the start of feeding with milk or artificial formula, lactobacilli and bifidobacteria are synthesized, which participate in the breakdown of milk sugar. Then the number of rods increases - Escherichia, Proteus, Klebsiella, and fungi appear. But despite this, the number of cocci, lacto- and bifidobacteria increases in such a way that they prevail over opportunistic pathogens. In some conditions, the opposite occurs, and the number of "harmful" bacteria prevails, which underlies the pathogenesis of dysbacteriosis. Normal colonization of the intestines occurs in a healthy mother who gave birth naturally and breastfeeds her child, and also eats properly. If any conditions are violated, this can cause the development of dysbacteriosis.
Today, given the difficult environmental situation, many births occur not naturally, but artificially. This can lead to the fact that the child, without passing through the birth canal, has more contact not with the mother's flora, but with the flora of the external environment, which is one of the risk factors for abnormal colonization of microflora. Among other risk factors, it is necessary to note artificial feeding of the child. After all, normal flora with a predominance of bifidobacteria and lactobacilli is formed during breastfeeding. If the child is fed with formula, then his composition of microorganisms is slightly different. And here it is also important what kind of formula the child is fed with, because if the formula is adapted, then it has the necessary probiotics and prebiotics, which prevents dysbacteriosis. Therefore, one of the risk factors for the development of dysbacteriosis is artificial feeding using non-adapted formulas. And further, speaking about the treatment of dysbacteriosis, an important role will belong to the correction of the baby's or mother's nutrition, if he is breastfed.
But the most common cause of dysbacteriosis is considered to be taking antibiotics. Of course, not all newborns are exposed to such influence, but if there are certain problems in the form of congenital pneumonia, inflammation of other localizations, then the prescription of antibiotics is mandatory and in fairly high concentrations. This leads to the fact that the still unstable microflora is exposed to antibacterial agents and the concentration of opportunistic flora increases.
One of the causes of dysbacteriosis can be considered the genetic characteristics of parents in terms of the functioning of the gastrointestinal tract. If one of the parents has chronic bowel diseases or functional disorders, then the child may begin to have problems already from the neonatal period, namely with the formation of an incorrect intestinal microbiocenosis. It has long been known that chronic inflammatory diseases of the digestive system in parents, which are etiologically associated with Helicobacter pylori, directly affect the composition of the intestinal wall microflora in their children. This also shows that there is a family connection between this disease of bacterial etiology and the development of dysbacteriosis in children. Violations of the ratio of pathogenic, opportunistic and normal microorganisms are often secondary in the case of damage to the digestive organs. Such primary pathologies include disaccharidase deficiency, cystic fibrosis, digestive disorders after surgery on the intestines or stomach (correction of pyloric stenosis in newborns), Meckel's diverticulum, congenital liver diseases or viral hepatitis, as well as pathologies of the stomach and intestines due to taking medications.
It is also worth noting other external causes of possible influence on the formation of intestinal microflora disorders. These include environmental factors such as air and soil pollution, disturbance of ecological biocenoses and the relationships between them, radiation and ionic radiation, as well as the state of food products and a healthy lifestyle. The nature of nutrition has a direct impact on the growth of a particular flora, because food that contains a lot of fiber and vitamins stimulates the active synthesis of prebiotics, and this in turn stimulates the growth of bifidobacteria. But more fatty foods inhibit all these processes and stimulate the growth of pathogenic flora. Fermented milk products maintain a normal amount of lactobacilli, which leads to the need for their daily consumption. These and other factors confirm the role of the mother's diet when feeding the child.
Internal factors that can influence changes in the content and ratio of flora are the following:
- pathology of the stomach, intestines, liver, pancreas with disturbances of their normal excretory and secretory functions;
- inflammation of the intestinal wall during acute intestinal infection or during chronic similar processes;
- the medicinal effect of drugs on the intestinal wall is direct or indirect through inhibition of the growth of normal flora, for example, uncontrolled use of antibacterial drugs;
- chronic diseases in a state of decompensation, when the intestines suffer due to ischemia or under the influence of toxins;
- a disease with an increased content of immunoglobulins of allergic etiology in newborns and children of the first year of life; a violation of the composition of normal microflora is also associated with insufficiently coordinated work of various organs and their response to such harmful environmental factors.
Therefore, when exposed to unfavorable factors, children are especially sensitive to such influences and it is necessary to identify risk factors in order to pay attention to this in advance.
Risk factors
Risk factors for the development of dysbacteriosis directly depend on the child’s age.
Dysbacteriosis in newborns often develops as a result of:
- pathological course of pregnancy and surgical interventions during childbirth;
- diseases of the genitourinary system in the mother in the form of cystitis, chronic ovarian infections;
- poor condition of the child after birth, which does not allow him to immediately be on the mother’s stomach and have contact with the skin;
- technical manipulations or resuscitation measures with damage to the mucous membranes and skin;
- staying in intensive care after childbirth and the risk of infection with “hospital” flora instead of home flora, as well as postponing early breastfeeding;
- physiological characteristics of a newborn baby and his unpreparedness for food;
- inflammatory and infectious diseases of the baby that require early long-term antibacterial therapy;
For children in their first year of life, the risk factors are as follows:
- incorrect social conditions and violations of basic nutritional rules and the correct introduction of complementary foods;
- transfer to formulas in early childhood with an unadapted composition;
- allergic skin diseases;
- digestive disorders due to pathology of the pancreas and liver;
- episodes of acute respiratory infections with antibacterial therapy without probiotic protection;
- concomitant diseases in the form of rickets, organic lesions of the nervous system, anemia, leukemia, immunodeficiency;
- children from disadvantaged families.
Risk factors in school-age children:
- improper nutrition with a predominance of harmful products and the formation of dietary rules that are later instilled in their children;
- the influence of propaganda of unhealthy diets and lifestyles;
- disorders of the sympathetic and parasympathetic nervous system with the formation of functional disorders;
- disturbances and shifts in the hormonal sphere in accordance with the age of the baby.
It is very important to remember that dysbacteriosis in a child is often a secondary process that occurs under the influence of certain factors that affect the normal state of the microflora.
Symptoms infant dysbiosis.
There is a concept of "transient dysbacteriosis" in a newborn. It includes those cases when in the first few days the child does not yet have a sufficient number of microorganisms and their normal composition. After all, some bacteria are populated only after two weeks or more, which is reflected in the child's stool. In the first 2-3 days after birth, the stool is green, with an unpleasant odor and thick. This is meconium, which contains particles of the epidermis, amniotic fluid that the child swallowed. Then, as the intestines are populated, the feces become transitional, and then normal - mushy. And the manifestations of such changes in the nature of the stool are transient dysbacteriosis, that is, a normal phenomenon in the first weeks after birth. Further, we will talk about a pathological process when this brings discomfort to the child.
The symptoms of dysbacteriosis are continuously connected with the main functions of intestinal microorganisms. And of course, the main function is the regulation of intestinal motility. Under the influence of microflora, a large number of prostaglandins and bradykinins are synthesized, which affect the contraction of the intestinal wall. Therefore, when this function is disrupted, problems with the tummy in infants in the form of spasms are observed, first of all. This leads to the fact that the child becomes restless, screams, and colic can develop against this background or as a consequence of such a disruption.
The first symptom that can alert in terms of the development of dysbacteriosis may be a change in the nature of the stool. This may be constipation in a newborn or, conversely, diarrhea. This happens because the process of digestion and digestion of basic food products is disrupted. When the feces become in the form of a chest - this is also considered abnormal, since for a newborn it should be mushy. But more often, with dysbacteriosis, loose stools develop in the baby, which should alert the mother. At the same time, the general condition of the child does not change, the body temperature remains normal.
The intestinal flora also takes part in the synthesis of vitamins and the implementation of the work of bile acids in the digestion of the main food particles. When the normal function is disrupted, the liver suffers secondarily, which is accompanied by allergic manifestations. Therefore, it often happens that all allergens are excluded from the newborn, the mother's diet is also ideal, but the allergy still remains. In this case, you need to consider that such manifestations are symptoms of dysbacteriosis. As a rule, this is manifested by the appearance of red rashes on the child's cheeks or spreading to the body. Such rashes are classically allergic.
Other clinical manifestations of dysbacteriosis include insufficient weight gain in the child. Since the disruption of the biocenosis disrupts the absorption of essential nutrients, the child may not receive enough kilocalories from food and not gain enough weight.
Complications and consequences
The consequences of dysbacteriosis in newborn babies can manifest themselves in the future in the form of a tendency to problems of the gastrointestinal tract of a functional nature. After all, if at the beginning the process of normal colonization of the intestinal microcenosis is disrupted, then in the future there will be constant problems in the form of intestinal colic, functional constipation or diarrhea, a tendency to food allergies. If dysbacteriosis is in a girl, then this often disrupts the composition of the flora in the genitals and, as a result, there may be problems with recurring infections of fungal and bacterial etiology.
Complications of dysbacteriosis in terms of serious pathologies occur very rarely. But if there are problems with absorption in the intestine, then the child may not gain weight with the development of protein-energy deficiency.
Diagnostics infant dysbiosis.
Most often, in the neonatal period, dysbacteriosis is a diagnosis of exclusion, since many functional diseases in children at this age can develop under the guise of dysbacteriosis. Therefore, there are conditions that can alert the mother, and even the doctor, in terms of possible dysbacteriosis in the child. If the baby has colic that does not go away after all elimination measures, and does not respond to the use of therapeutic agents, then perhaps you should think about the problem with the intestinal biocenosis. Also, protracted allergic manifestations that cannot be corrected can be caused by the same problem.
Based on this, the diagnosis of dysbacteriosis is a little difficult at the stage of complaints only, since they can be very diverse. But most often there are problems with the stool - this is diarrhea or constipation with a change in the nature of the stool, the appearance of solid undigested particles or a change in color. At the same time, the child may have bloating or rumbling, which is accompanied by anxiety.
During the examination, no specific diagnostic signs of dysbacteriosis can be seen, and only additional examination methods can accurately establish such a problem. Children with dysbacteriosis as a primary diagnosis have a healthy appearance, good weight, they are active and correspond to the development of their age. If any problems are visible during the examination, then we may be talking about primary organic pathologies, against which dysbiosis is already developing.
Laboratory tests of feces are always necessary for an accurate diagnosis. Feces analysis is also performed for the purpose of differential diagnostics, so a study is conducted for dysbacteriosis, as well as a coprogram. A coprogram is an analysis that allows you to evaluate the secretory function of the intestine. But the presence of a small amount of undigested fiber or other substances can be normal for a newborn due to the immaturity of its enzymatic function.
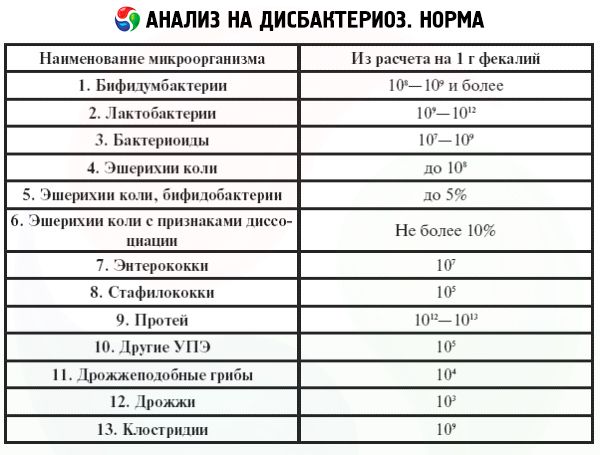
Dysbacteriosis tests in newborns are informative only if the technique is correct. How to submit a stool sample for dysbacteriosis in a newborn? First of all, the stool should be fresh, in some cases they say warm. This is true, because even “good” bacteria live outside their environment only for a certain time. The container for collecting stool must be sterile, because the content of other microbes there can affect the result. Well, the collection technique itself must provide for all the rules of hygiene. These are the basic requirements for collecting such a sample. The results of the analysis provide for an indication of all the microbes that are in the stool. Under normal conditions, the total amount of intestinal flora is determined in a healthy child, as well as the number of E. coli, streptococci, hemolytic and non-hemolytic strains of staphylococci, fungi. An increase in the number of these bacteria indicates not only dysbacteriosis, but also an active infection with a predominance of certain bacteria. The analysis also determines the amount of lactobacilli and bifidobacteria, and if they are less than normal, this indicates the benefit of primary dysbacteriosis.
Instrumental diagnostics are not performed, since there is no organic pathology.
What tests are needed?
Differential diagnosis
Differential diagnostics of dysbacteriosis should be carried out primarily with pathologies that arise due to absorption disorders and are accompanied by changes in the child's stool. Disaccharidase, primary lactase deficiency, gluten enteropathy, cystic fibrosis are diagnoses that must be excluded first of all in an infant.
Lactose deficiency may have symptoms that may initially resemble the course of dysbacteriosis. This is manifested by regurgitation, bloating, colic, diarrhea, underweight, and poor health of the child.
Therefore, it is essential to clarify during differential diagnostics whether there are any stool characteristics in relation to a certain food.
Who to contact?
Treatment infant dysbiosis.
A very important stage in the treatment of dysbacteriosis is proper nutrition. And if we are talking about the fact that the main nutrition for a child is breast milk, then it is very important what exactly the mother eats.
Infants fed exclusively on mother's milk develop a specific flora during the first week after birth, which becomes dominant by the end of the first month of life. The infant's primary flora is the flora of the mother's birth canal and colon.
The combination of an acidic environment (lactic acid), probiotics and prebiotic factors (bifidofactor, lactoferrin, casein and nucleotides) leads to the formation of flora by the end of the first month, in which lactobacilli and bifidobacteria predominate. Therefore, the mother's diet not only affects the quality of milk, but also the functional activity and motility of the child's intestines. There are certain foods that a nursing mother should exclude from her diet, which may be the only treatment for dysbacteriosis in her child even without the use of medications. The mother must exclude all spices from the diet with limited salt, as well as fried foods. You cannot drink whole milk, at least in the first month of the child's life. The need for calcium and phosphorus can be met by cottage cheese and kefir, which should be no more than 250 grams per day. Coffee should also be excluded, only green tea without any additives. It is clear that chocolate and sweet bakery products should also be excluded. The diet should contain a sufficient amount of vegetables and fruits. These are general recommendations for the mother's diet, which the doctor can adjust taking into account certain problems.
Newborns fed with formula have a large number of enterobacteria and gram-negative organisms in their flora. This is a consequence of the alkaline environment and the absence of prebiotic factors. That is why if a child is bottle-fed, he needs additional probiotics and prebiotics in his diet to avoid the development of dysbacteriosis or to correct it if it has already developed.
Infant formulas for dysbacteriosis must necessarily contain substances that normalize the intestinal microflora. First of all, if the child is bottle-fed and receives some kind of formula, it must be adapted. This word means that it contains probiotics in sufficient quantities to prevent the development of dysbacteriosis. Adapted formulas include: Malutka Premium, Bellakt, Frisolac, NAN, Nestozhen, Hipp. There is another aspect - if the child has already developed dysbacteriosis, it is better to choose a formula with the maximum amount of prebiotics and probiotics. The prebiotics that are most often used in formulas include fructooligosaccharides and galactooligosaccharides. These substances, entering the child's intestines, are the nutrient medium on which the bacteria grows, which is so necessary for the child with dysbacteriosis.
When choosing a formula, you need to consider the manifestations of dysbacteriosis that the baby may have. For example, if the baby regurgitates, you need to take an anti-reflux formula (HUMANA anti-reflux) and give it to the baby in a small amount, for example, 20 grams, at the beginning of feeding. Then you need to give the main part of the regular formula.
If the baby's dysbacteriosis manifests itself as diarrhea or constipation, or there are colics against the background of dysbacteriosis, then the NAN Triple Comfort mixture is suitable.
Only a doctor can know such nuances when choosing a mixture, so it is important to address such a problem in order to solve it correctly.
Drug correction of dysbacteriosis in a newborn is usually always used, since it is very important to restore the correct composition of the child's intestinal microflora. There are many probiotic drugs, and to understand them, you need to know the main groups of such drugs.
- Probiotics are microorganisms that, when ingested, can have a positive effect and help prevent and treat a specific pathological condition, in this case, dysbacteriosis. As a rule, they are of human origin. These microorganisms are not pathogenic and not toxicogenic, and remain viable during storage. They survive to a certain extent when passing through the stomach and small intestine. Probiotics can create colonies on the surface of the mucous membrane outside the gastrointestinal tract, and when taken orally, they help maintain the health of the oral cavity and genitourinary system as well.
- Prebiotics are non-digestible substances that, when ingested, selectively stimulate the growth and colonization of beneficial probiotic bacteria normally found in the intestines. These include fructooligosaccharides (FOS) - such as chicory or inulin - as well as lactulose, lactitol, and inulin.
- There are also synbiotics - a combination of prebiotics and probiotics in one drug. This is the most optimal combination for complex treatment.
There are also groups of probiotics by generation and composition:
Single-component (Lactobacterin, Bifidumbacterin) are practically not used today due to their narrow spectrum of action.
- 2nd generation - a combination of bacteria with yeast fungi and bacillus spores (Enterol, Biosporin) - they are used in limited cases for intestinal infections.
- 3rd generation – combined (Linex, Bifiform, Lactiale) – most often used in antibacterial therapy and in a number of other cases.
Which combine a probiotic and activated carbon or other substance. They are not used daily in pediatric practice.
The main medications that are most commonly used are:
- Acipol is a drug that belongs to the group of synbiotics. It contains acidophilic bacteria and fungi. Fungi are prebiotics, as they are necessary for the normal growth of bacteria. The mechanism of action of the drug in dysbacteriosis is to activate acidobacteria, which suppress the growth of pathogenic microorganisms. It also stimulates the synthesis of fatty acids in the intestine, which changes the pH in the intestine and additionally inhibits the growth of pathogenic flora. Motility and peristalsis are also stimulated due to the active work of kefir-like fungi. This leads to normal bowel movements of the child and to an improvement in the entire digestion process. The method of using the drug for the treatment of dysbacteriosis is one capsule three times a day for at least seven days. For prevention, use one capsule per day for two weeks. Side effects are observed in the form of a change in the nature of the stool, the appearance of diarrhea - which requires a change in dosage. Precautions – the use of any probiotics is not recommended for children with septic conditions.
- Biosporin is one of the most commonly used probiotics today. The drug contains two main strains of live bacteria Bacillus subtilis, Bacillus licheniformis. In case of dysbacteriosis in a newborn, they create conditions for restoring the baby's own intestinal flora, and help normalize the qualitative composition of bacteria in the baby's intestines. In a newborn, the drug restores a sufficient amount of bifido- and lactobacilli, as well as E. coli in case of dysbacteriosis. The method of using the drug for newborns can be in the form of a sachet or in bottles. The dosage of the drug for treatment is one dose (in the form of a sachet or in a bottle) per day. The drug should be dissolved in a teaspoon of milk or formula and given to the child. The duration of therapy is about 10-15 days. Side effects when using the drug were not detected.
- Enterol is a drug used to treat dysbacteriosis that develops against the background of long-term antibacterial therapy and is accompanied by diarrhea. The drug contains yeast-like fungi Saccharomycitis bullardii, which exhibit an antagonistic effect on many pathogenic microbes involved in the development of dysbacteriosis in a baby. Fungi also neutralize toxins that are released in the intestines and disrupt its normal functioning. The drug reduces the severity of diarrhea due to its direct action. The method of using the drug for newborns is best to use a sachet. One sachet per day once for seven days. Side effects can be such as constipation.
- Linex-baby is a probiotic preparation, which includes bifidobacteria, which act on pathogenic microbes and reduce their activity in case of dysbacteriosis. Bifidobacteria are representatives of the normal flora of a newborn from the first hours of his life, therefore, a sufficient amount of them helps to restore the flora that is lacking in case of dysbiosis. The most convenient way to use the preparation is in the form of a sachet. To treat dysbacteriosis, it is necessary to use one sachet per day, dissolving it in milk or formula. Side effects may occur in children with immune reactions in the form of rashes, itching.
- Bio-gaia is a probiotic that is actively used to correct problems associated with dysbacteriosis in newborns. The drug contains active strains of the Lactobacillus reuteri bacteria, which help improve the condition of the intestines by synthesizing lactic and acetic acids. These acids suppress the growth of many pathogenic microbes and thus restore normal flora. The method of using the drug is 5 drops per day, adding them to the mixture or breast milk. Dysbacteriosis is treated for ten days. Precautions - the drug may contain vitamin D, which should be taken into account already during the prevention of rickets to prevent an overdose of vitamin D.
- Prema is a drug from the group of synbiotics, which contains prebiotics in the form of fructooligosaccharides and probiotic Lactobacillus rhamnosus GG. This drug, getting into the baby's intestines, immediately begins to work due to the content of the prebiotic. It inhibits the reproduction of pathogenic bacteria and prevents their further growth. The method of application for newborns in the form of drops - ten drops per day, dissolving them in milk. Treatment can be carried out for two to four weeks. Side effects were not observed.
Vitamins in the treatment of dysbacteriosis can only be used in the mother's diet if she is breastfeeding. After all, some vitamins are needed for the normal functioning of the intestinal flora. For this purpose, nursing mothers can only use vitamins for pregnant women, which are tested accordingly.
Physiotherapeutic treatment of dysbacteriosis in newborns is used only in isolated cases. Most often, when dysbacteriosis develops after surgical interventions on the stomach or intestines of the child, then there may be a need for such therapy only during the rehabilitation period. In the acute period and with primary dysbacteriosis, physiotherapy is not used in infants.
Very often mothers wonder whether it is possible to cure dysbacteriosis in a baby without using a lot of medications. After all, there are baby yogurts, kefirs, which contain natural beneficial bacteria. The answer here is unambiguous - dysbacteriosis can be prevented, but it cannot be cured. All this is because, firstly, newborns cannot be given anything except formula and milk, even baby yogurts are allowed as complementary foods from eight months. Secondly, they contain a very small number of bacteria, which is not able to compete with a huge number of pathogenic ones. For treatment, there must be a concentration of bacteria of a certain type in a certain volume. Therefore, the use of probiotics in the treatment of dysbacteriosis is a priority. That is why folk methods of treatment, herbal treatment and homeopathic drugs are not used in this case. On the contrary, all these methods can only additionally burden and allergenize the child's body.
Prevention
Prevention of dysbacteriosis in a newborn is, first of all, breastfeeding, because breast milk contains as many prebiotics and probiotics as the baby's body needs. If the baby is bottle-fed, then it is necessary to choose a highly adapted formula for him, which is as close as possible to breast milk. It is important in the prevention of dysbacteriosis to correctly form the baby's microflora immediately after birth, so the mother needs to have all the conditions for an ideal pregnancy and childbirth.
Forecast
The prognosis for dysbacteriosis is positive with proper correction, although it can cause a lot of discomfort for the baby. Speaking about potential risks, with dysbacteriosis in the neonatal period, the prognosis for allergic reactions in such a child is higher than in others, so it is important to take this into account in the future.
Dysbacteriosis in a newborn is a violation of the normal composition of the flora of his intestines due to exogenous or endogenous causes. In this case, the normal processes of digestion, peristalsis, absorption are disrupted, which is manifested by stool disorders, colic. Correction of this condition is complex - these are medications and the diet of the nursing mother or the composition of the mixture for feeding the child.


 [
[