Medical expert of the article
New publications
Ureaplasma
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
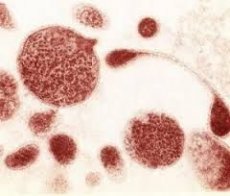
Ureaplasma is an inhabitant of the microflora of the urinary tract, but it is far from permanent.
In fact, it is a conditionally pathogenic microorganism that can be found in the organs of the urinary system and does not cause any symptoms. On the other hand, in case of exposure to a certain provoking factor on the human body, being infected with ureaplasma, ureaplasma infection can be activated.
In the pathogenesis of the disease the leading role is played by the inflammatory process, which develops as a result of the vital activity of the ureaplasma. There are several ways of infection by this pathogen - it's the sexual way and the vertical one. The latter includes infection of the fetus from the mother during pregnancy or during labor.
For the first time about ureaplasma they began talking in the middle of the 20th century, when they discovered an unknown microorganism in a patient with a non-neoconial urethritis origin. The microorganism was characterized by small sizes slightly exceeding the viruses, as well as the absence of the cell membrane and its own DNA. A typical location of ureaplasma is the mucosa of the urinary tract and genital organs.
Ureaplasma Parvum
Ureaplasma parvum (parvum) belongs to the family of mycoplasmas, in particular to ureaplasmas. The size of the microorganism is very small, but urease activity is quite pronounced. This property provides the ability to cleave urea with the release of ammonia. As a result, there is a threat of the development of an inflammatory reaction and the formation of stones in the organs of the urinary system.
The habitat of ureaplasma is the cells of the body, in view of the fact that they do not have their own membranes. As a consequence, the pathogen is connected to the cell membranes of the mucous membranes with further destruction.
In addition, ureaplasma is able to produce enzymes that have the property of provoking the destruction of proteins, namely, immunoglobulin A. This choice is justified by the ability of the protein to produce antibodies in response to the action of pathogens tropic to mucosal cells.
Having destroyed the protection of cell membranes, ureaplasma Parvum freely penetrates into the cell due to a decrease in local immunity.
Ureaplasma urealitikum
Ureaplasma urealyticum (urealyticum) is an intracellular microorganism that belongs to mycoplasmas. This type of bacteria is distinguished by the absence of a cell membrane and DNA.
The causative agent is considered a conditionally pathogenic inhabitant of the microflora of the genitourinary tract, however, despite this, it refers to infections transmitted through sexual contact.
Ureaplasma urealitikum under the influence of certain factors on the weakened organism can provoke the development of the inflammatory process in the urinary and genital system, as well as affect the joints. More than 40% of people are carriers of ureaplasma and do not even know about it. This situation is due to the lack of activity of the causative agent and, accordingly, clinical manifestations of the disease.
Due to the fact that drug therapy of ureaplasma during pregnancy can adversely affect the development of the fetus, therefore it is recommended to conduct a laboratory test for the presence of this pathogen when planning pregnancy. The analysis should be conducted at both future parents and at detection of a ureaplasma - to spend treatment.
Ureaplasma hominis
Ureaplasma hominis (hominis) refers to mycoplasmas, which have a similar structure with ureaplasmas and are intracellular parasites. The size and shape of the pathogen can vary, but their common feature is the three-layer cytoplasmic membrane.
Ureaplasma hominis after introduction into the host cell contributes to the development of serious disorders in protein metabolism, its synthesis, the formation of nucleic acids, and also alter the genetic information.
Propagation of the pathogen occurs by dividing the mother cell or by budding the daughter cells from it.
The risk of infection with ureplasma during or before pregnancy, without any clinical manifestations, may be the initiation of spontaneous abortion, premature birth, the birth of a dead fetus, or pathological conditions during pregnancy or labor.
This threat is due to the ability of the pathogen to increase the volume of arachidonic acid in the free state, which in turn leads to activation of prostaglandin production.
Ureaplasma Genitalia
Ureaplasma genitalium (genitalium) is part of the mycoplasmas family, which belong to intracellular pathogens. After entering the cells of the mucous membrane of the urogenital system, mycoplasma begins to process such host cell substances as fatty acids and cholesterol.
The ability to attach an intracellular parasite has not yet been fully elucidated. Only it is known that after binding of mycoplasmas to the urethral epithelium a rather strong connection is formed that does not burst under the pressure of the urine stream.
However, in the process of microscopic examination with the help of an electron microscope, it was established that the ureaplasma of the genitalia does not have direct dense adhesion to the host cell membrane.
There are not many pathways of infection-sexual and vertical, but nevertheless the most predisposing factors are identified for infection with ureaplasma. These include the age category from 14 to 30 years. In addition, the early onset of sexual activity (up to 18 years), disorderly change of partners, as well as the transferred gynecological pathology in the form of tubal pregnancy, sexual infections and chronic inflammatory processes of unknown origin.
Symptoms of ureaplasma
The duration of the period from the moment of getting ureaplasma into the body before the appearance of the first clinical signs can pass from several days to a month. This period depends on the immune defense of the human body, as well as on the degree of pathogenicity of the pathogenic microorganism.
The incubation period can last even more than a couple of months, during which the person is already infected and is the source of infection. Thus, at this stage, infection of the sexual partner may occur at an asymptomatic stage.
Symptoms of ureaplasma start to appear not very noticeably, in connection with which it is impossible to accurately determine the moment of infection and the duration of the incubation period.
In some cases, clinical manifestations of the disease can be so worn out that a person will not even suspect of their infection and infection of the sexual partner. This is especially true of the female half of humanity, in which the ureaplasma infection can be virtually asymptomatic for decades.
Symptoms of ureaplasma in women
At a normal level of immune defense of the body, ureaplasma women may not show themselves for a fairly long period of time. However, as soon as the organism is exposed to any provoking factor, when a secondary infection or the development of concomitant pathology is attached, the ureaplasma begins to remind of its presence.
In addition, pregnancy may become such a starting moment, which in the future does not allow to apply the entire medicinal spectrum of drugs, which is necessary for the death of ureaplasma.
Symptoms of ureaplasma in women are characterized by the presence of vaginal discharge, the color of which is usually clear and does not have a specific odor. However, it is worth remembering that with the development of the inflammatory process, the discharge can acquire a yellowish or greenish hue, as well as an unpleasant odor.
The localization of inflammation in the uterus or appendages can indicate painful sensations of the pulling character in the lower abdomen. In the case of the oral-genital route of infection, it is possible to develop inflammation of the oropharynx with pain syndrome and purulent deposits on the tonsils.
In addition, the symptoms of ureaplasma in women are manifested by frequent urge to urinate, which is accompanied by a burning sensation and pain in the course of the urethra. Also, pain and discomfort can accompany sexual intercourse.
Symptoms of ureaplasma in men
Symptoms of ureaplasma in men begin to manifest themselves with negligible severity. In most cases, the disease is not found in the first months of infection. The most frequent clinical manifestations are burning in the urethra during the act of urination.
Often, there may be mucosal discharge, which, in combination with other symptoms, may periodically arise and disappear for no apparent reason.
Not paying due attention to the disease, it can go into a chronic course, which will exacerbate the situation, since it is much worse treatable. In addition, it is possible to involve the appendages of the testicle and prostate in the process, which leads to infertility.
Symptoms of ureaplasma in men with urethral lesions are manifested by cutting pains, burning and discomfort in the area of the urethra. These clinical manifestations are troubling during urination and can disappear on their own. In chronic course, each subsequent exacerbation has more pronounced symptoms.
Epididymitis is not manifested by any symptoms, but leads to an increase in the appendages, which acquire a dense consistency. Prostatitis is considered as a complication of uraplasmal infection and is characterized by difficulty with urination, frequent urges and uncomfortable sensations in the perineal region, which further contributes to erectile dysfunction and the development of impotence.
Diagnosis of ureaplasma
Diagnosis of ureaplasma is based on the same principles in women and men, but nevertheless there are some nuances. For diagnosis of ureaplasma in men, it is necessary to conduct an examination of the external genitalia, palpation of the scrotum, including the epididymis, testicles and the spermatic cord.
Next, you need to examine the prostate gland and seminal vesicles through the rectum, that is, rectally. Among the laboratory and instrumental methods of examination, a microscopic examination of a urethral smear, a urinary sediment of a 2-glass sample, and a secretion of the prostate should be distinguished.
In some cases, spermiogram and ultrasound examination of the structures of the scrotum and prostate gland is required.
Diagnosis of ureaplasma with infection of women consists of external and internal examination of the vaginal mucosa, its walls and cervix. Using bimanual examination, it is necessary to feel the uterus and appendages, determining the soreness, consistency and size.
From microscopic methods, isolate the urinary sediment, a smear from the urethra and cervical canal and vagina. Instrumental methods include ultrasound of the organs of the female reproductive system, as well as laparoscopy if necessary.
 [1], [2], [3], [4], [5], [6], [7]
[1], [2], [3], [4], [5], [6], [7]
Analysis for ureaplasma
The analysis for ureaplasma is performed after the gynecologist (in the case of a woman's treatment) or the urologist (for men) will inspect the genitals, palpatory examination of the structures available for this procedure, and also with the help of an anamnesis of the disease find out the factors that could cause infection with ureaplasma.
Analysis for ureaplasma is carried out with several purposes.
First, this is the definition of the causative factor, which became the starting point in the development of the chronic inflammatory process in the urogenital system.
Secondly, additional research is necessary in the absence of the use of barrier contraceptives, as a result of which infection with ureaplasma during sexual intercourse can occur. In addition, the frequent change of sexual partners is also an indication for a more thorough examination.
Thirdly, tests for the detection of ureaplasma are needed in planning pregnancy in order to avoid infection of the fetus or the development of the disease in this period. Quite often ureaplasma is identified as the cause of infertility, as well as with ectopic pregnancy.
And, at last, the analysis can be carried out with the preventive purpose in order to avoid the development of the disease and the infection of its sexual partner.
 [8], [9], [10], [11], [12], [13]
[8], [9], [10], [11], [12], [13]
Sowing on the ureaplasma
Of all the tests performed to diagnose a pathogenic pathogen, it is worth highlighting the sowing for ureaplasma. It is considered the most accurate, so it is used most often. This study is also called a bacteriological or cultural diagnostic method.
In order to carry out sowing on the ureaplasma, it is necessary to first take smears from the mucous vaults of the vagina, cervix or from the urethra. It is possible to carry out a bacteriological study with the help of morning urine.
After collection of the material, it is placed on a suitable nutrient medium, where the ureaplasma will be grown. In addition to the growth of the pathogen it is necessary to evaluate the quantitative composition. This requires bacteriological inoculation.
In addition, it can help not only to count the number of microorganisms, but also to determine their sensitivity to antibacterial agents, which in many ways facilitates the process of treatment. Thanks to this method, it became possible to use drugs purposefully, which will lead to death of the ureaplasm.
PCR ureaplasma
PCR is the most informative method for determining a pathogenic agent in the discharge from the vagina or urethra. This type of study is a molecular diagnosis of infectious agents that are transmitted through sexual contact.
With the help of PCR ureaplasma, or rather its DNA, is detected even if there are only a few units in the smear. Correct analysis provides 100% accuracy.
Using PCR, ureaplasma and other sexual infections are detected in a minimal amount, which makes it possible to distinguish this method among others. Particularly relevant is the conduct of PCR in the hidden course of the disease, as well as in cases where other methods can not identify the pathogen.
Thanks to PCR, pathogens are accurately determined even in the chronic and slow flow of the disease. In this regard, ureaplasma can be diagnosed at the stage of the incubation period, which prevents infection of the sexual partner.
Also, the method is widely used in the negative results of laboratory testing and the absence of clinical manifestations.
Titres of ureaplasma
The titres of the ureaplasma are determined by PCR or culture on a nutrient medium. The result of the first analysis will be the degree of activity of microflora, and the second - the quantitative composition and sensitivity of the pathogen to antibacterial agents. Thanks to the latter, treatment is more effective, since antibacterial drugs are used that can lead to ureaplasma death.
The indication of the titer from 101 to 104 implies the presence of ureaplasma in the material taken, but it is not a basis for carrying out the therapeutic drug course. Titer 101 can be observed in the female body when the disease was treated, but not until the end. In the process, the ureaplasma passed from the pathological flora to the normal one.
Indicators 102 and 103 indicate the presence of ureaplasma as a conditionally pathogenic microorganism, which does not require treatment. However, in the presence of clinical symptoms or when a disease is detected in the sexual partner, a further examination is needed and it is most likely to undergo a therapeutic course.
Ureaplasma titers - 104 and more mean the activity of the disease, so in this case it is necessary to carry out treatment. However, there may not be clinical manifestations, but in the future ureaplasma can cause infertility.
Treatment of ureaplasma
Treatment of ureaplasma involves the use of several groups of drugs, as well as compliance with certain rules. Treatment should be carried out simultaneously by both sexual partners. It consists of antibacterial agents, to which the microorganism is sensitive. This course should be continued for up to 2 weeks.
In addition, you need to use immunostimulating drugs to increase the body's defenses. Of the local methods of treatment is to highlight the introduction of the urethra of special medicines, for example, uroseptics. This procedure was called installation.
Treatment of ureaplasma also implies the use of physiotherapeutic procedures, and in the case of prostatitis, as complications of ureaplasma infection, even in combination with prostate massage.
During the treatment, you should stop having sex and follow a special diet. Control over the dynamics of the therapeutic course is carried out using PCR. This analysis is applied several times within 3-4 months.
Sensitivity of ureaplasma to antibiotics
The sensitivity of ureaplasma to antibiotics is established by the culture method, when an antibacterial agent is identified that has the maximum effectiveness in fighting this type of pathogen. Treatment should be started when clinical signs of the disease appear, as well as when the titer exceeds 104 as a result of PCR.
First, a list of groups of antibacterial drugs should be listed, to which the ureaplasma is absolutely insensitive, so their use will not have any effect. These include cephalosporins, rifampicin and penicillin.
The sensitivity of ureaplasma to antibiotics of such groups is proved: macrolides, tetracyclines, lincosamines, fluoroquinolones and aminoglycosides. However, certain doses of drugs should be taken into account, because even effective antibiotics in insufficient dosage can not contribute to the death of ureaplasma.
So, for the treatment of ureaplasma, it is rational to use doxycycline (Unidox Solutab), but it is contraindicated and up to 8 years old. The same contraindications have a representative of fluoroquinolones - oflocacin.
From macrolides it is necessary to allocate josamycin, erythromycin, midecamycin, azithromycin and clarithromycin. The first has good tolerability and can prescribe in the first trimester of pregnancy, as well as the next two antibiotics.
As for clarithromycin and azithromycin, they have a high ability to penetrate into the cell, but are contraindicated in pregnancy.
Preparations for the treatment of ureaplasma
The complex treatment of the disease includes physiotherapeutic procedures, installations, as well as drugs for the treatment of ureaplasma.
Antibacterial drugs are the drugs of choice, since without them the death of ureaplasma is impossible. For this purpose, macrolides, tetracyclines and fluoroquinolones are widely used, to which the causative agent is sensitive. The form of antibacterial drugs can change, so you can use tablets in the form of powders, solutions or suppositories. In addition, if necessary, rational use of metronidazole as an antifungal agent.
Immunotherapy includes the use of immunostimulants, since ureaplasma infection is observed in most cases in people with insufficient level of immune defense of the body. Such drugs are needed for rapid recovery. Among them, preference is given to Cycloferon.
In addition, from the rehabilitation therapy should be allocated such drugs for the treatment of ureaplasma, as antioxidants, adaptogens and biostimulants.
Ureaplasma refers to infections that are sexually transmitted, therefore, when the first clinical manifestations of the disease appear, you should immediately contact a specialist. Early detection and treatment will prevent infection of the sexual partner and the transition of the disease to a chronic form, which entails serious consequences.

