Medical expert of the article
New publications
Toxic hepatitis of the liver: acute, chronic, drug, alcoholic
Last reviewed: 18.10.2021

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
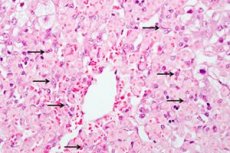
Under toxic hepatitis should be understood pathological process in the liver, which occurs as a result of the fact that the body penetrates toxic substances. Since their main processing and neutralization occurs precisely in the liver, in connection with which develops an inflammatory process of acute or chronic nature. Toxic hepatitis in the acute form occurs as a result of the penetration of a high concentration of toxin into the body, which breaks the structural and functional disorder of the liver. In chronic hepatitis, the body is permanently and permanently affected by damaging agents, the pathology is worsened gradually.
First, liver cells are damaged, then death occurs. The tissue is gradually transformed and replaced by a connective tissue. This is associated with functional disorders, pain in the liver. Progression of jaundice.
If the disease in time to begin to heal, you can slow or stop the development of the disease. If you do not take any effort, you can get serious complications, up to cirrhosis, severe insufficiency, which often result in death.
Epidemiology
Analyzing the statistical data, they found that liver damage is more affected by women than men. The earlier the therapy will be, the outcome of the disease will be better. The occurrence of bleeding is the cause of death in about 30-50%. Coma has a lethal outcome in 80-100%. The appearance of ascites ends in a lethal outcome of 80%, death occurs within 3-4 years.
Causes of the toxic hepatitis
Hepatitis can develop in the event that the body gets toxic substances. Such a hit can be accidental or intentional. For example, they often poison poisonous mushrooms, taking them for edible. Professional activity is often associated with accidental poisoning. While working with toxic substances, acids, vapors and dust gets into the human body and has a damaging effect. Intentional poisoning is a case of suicide, in which a person uses poison inside.
The main way of penetration of toxins into the liver is oral, through the digestive tract. From the stomach occurs absorption, then transportation. In the hepatic tissue have a major damaging effect.
The cause of poisoning can be long-term use of medications, or their high dosages. The greatest danger is represented by drugs acting against viruses, seizures, and also isoniazid.
Substances that are used in production can also poison the liver. In this case, the liver can be subjected to acute or chronic pathology. All this is accompanied by the death of the liver. The greatest danger is represented by phenolic compounds, arsenic, phosphorous elements. The reason may be the abuse of alcohol, especially if it is substandard, drugs. This is due to the fact that the main processing is laid on the liver. The danger of toxic effects is caused by a violation of fat metabolism: there is a fatty degeneration of liver cells. Narcotic elements are also neutralized. Many weeds and fungi have a toxic effect.
Risk factors
People who are professionally involved in toxins and corrosive components are at risk. Alcoholics, drug addicts often end up living with liver diseases. Suicides who have taken poison for the purpose of suicide, but survived, already have severe liver damage, which can progress.
People who are forced to constantly take potent medicines should monitor the liver. Especially it concerns those patients who take painkillers, anti-tuberculosis drugs. If a person already has any liver disease, viral hepatitis or he is a carrier of viral hepatitis, he automatically falls into a risk group. In the elderly, the risk of developing significantly increases, as the liver does not cope with the load and processes everything much more slowly. Women are more at risk than men. This is due to a lower level of metabolism. Toxins in women are excreted much longer than in males.
Heredity plays an important role. There is a genetic predisposition to the development of liver diseases. Possible possible abnormalities in the structure of the liver, functional disorders are also taken into account. In addition, improper generation of enzymes can not only inhibit the neutralization of toxins, but also stimulate their additional synthesis in the body. Also today, people who practice non-traditional types of intimate relationships and people with non-traditional orientation fall into the risk group.
Pathogenesis
At the heart of pathogenesis is the damaging effect of toxins on the human body. There is a defeat of hepatocytes, structural and functional disorders, further dying off and replacement with adipose tissue.
There is also a second mechanism for the development of pathology. In the liver, microcirculation of the blood can be disturbed. There is a damage to the vascular bed, as a result, the supply is broken, the body does not receive the necessary amount of nutrients, oxygen. High concentrations of exchange products and carbon dioxide accumulate. It damages the liver, it has a toxic effect on it. Violated metabolic processes in the liver, including oxidation-reduction. Carbohydrate and protein metabolism suffers. Gradually, even the composition of blood. This causes irreversible processes in the cell membranes: DNA replication is broken, enzyme activity is reduced, respiratory processes are inhibited. Hepatocytes undergo dystrophic processes and gradually die off.
The third way of violations is associated with a violation of normal bile acid metabolism, as a result of which bile exchange is disturbed, blood flow velocity in the bile capillaries decreases, and bile flow out through the intrahepatic bile ducts decreases. The result is the same as in the first two cases: hepatocytes are damaged, their degeneration and gradual withering take place.
How is toxic hepatitis transmitted?
Many are worried about not infecting their relatives and family members with toxic hepatitis. It can be safely assured: there is no cause for concern. Cases of family development of hepatitis are not possible. Exceptions are cases of eating poisonous substances (for example, fungi), or spoiled food. The path of transmission through contacts and household things is excluded.
Symptoms of the toxic hepatitis
Usually hepatitis can be recognized by painful sensations under the right rib. Most often, the pain manifests itself on the 2-5th day. The liver is enlarged. It shows a muscle weakness. Acute process is accompanied by intensive bleeding, bleeding gums, brittle vessels and small bruises on the skin surface. Also, human behavior changes significantly: becomes overexcited, or vice versa, pathology manifests itself in a slow reaction. Gradually joins a shiver in the body, a gradual loss of weight. Periodically the stomach is swollen, diarrhea appears. This is caused by a violation of the outflow of bile. Sharply decreases working capacity, fatigue increases. An important sign is itching all over the body. The skin begins to itch as a result of increasing the amount of fatty acids in the dermis of the skin. The liver and spleen increase in size. Chronic hepatitis indicates alternation of periods of remission and exacerbation.
Once you notice the pain in the liver (under the right rib), you need to see a doctor as soon as possible. Also, the early symptoms include a decrease in appetite, dyspeptic disorders.
Itching of the skin with toxic hepatitis
Skin itching is caused by the accumulation of bile acids in the lower layers of the skin. To prevent this unpleasant phenomenon, it is necessary to drink hepatoprotectors, which protect the skin from harmful effects.
Exacerbation of toxic hepatitis
There is an alternation of the period of remission, in which the person is well-being with well-being, with exacerbations. Exacerbation is accompanied by digestive disorders, an increase in the liver to such a size that it can be safely probed under the right rib. The temperature may rise, intoxication occurs.
 [21], [22], [23], [24], [25], [26]
[21], [22], [23], [24], [25], [26]
Toxic hepatitis in pregnancy
The development of hepatitis in a pregnant woman is indicated by pain in the liver, fever, bleeding and bleeding. Behavior changes dramatically: retardation or increased excitability develops. Possible loss of consciousness. Increases not only the liver, but also the spleen, there is a skin itch.
When the first signs appear, it is important to consult a doctor immediately for the correct diagnosis and selection of treatment. Self-treatment is strictly prohibited. A pregnant woman should follow a strict diet. You should also keep bed rest. Detoxification therapy is carried out, absorbents are applied. Hepatoprotectors and cholagogue preparations contribute to the recovery of liver cells. In severe cases, antidotes are used.
In order to prevent pregnancy, it is necessary to plan pregnancy in advance, to be checked in advance. It is important to cure any liver disease, even if they are in a state of remission or proceed in a latent form, and do not bother the woman at all. Otherwise, inflammation can not be avoided. In the presence of liver disease in history, you need to regularly check, undergo a survey.
For pregnant women, toxic hepatitis is especially dangerous for its complications. Develops hepatopathy, as a result of which blood clotting is disrupted. This is dangerous in childbirth, as it increases the risk of bleeding. With the development of such complications, in most cases, coagulopathic therapy is carried out, after which the pregnancy is interrupted, treatment is continued. No less dangerous complication is hypercoagulability, in which coagulability increases. This is fraught with the formation of blood clots. Both pathologies require abortion. Delivery is accompanied by hepatoprotective therapy, infusion of fresh frozen plasma, stimulation of hemostasis. All pregnant women with liver damage of any etiology require urgent hospitalization.
Toxic hepatitis in children
Toxic liver damage in children is rare. If we analyze those rare cases of defeat, it can be noted that neurologic and cardiorespiratory symptoms prevail in such children. Develops circulatory disorders of the liver. Most often, children experience occasional poisoning, namely poisoning with a pale toadstool. Less often observed ingestion of a large concentration of drugs or toxic substances. Children use them in ignorance because of excessive curiosity, if the parents have hidden the poison far from the child. The child is immediately sent to the intensive care unit, as acute necrosis develops dramatically.
In children, unlike adults, lesions can be due to allergies, severe impairment of the immune system. They appear more heavily. Children, in addition to traditional symptoms, can experience anaphylactic shock, intense skin rashes, immune system disorders, including immunodeficiency. Diuresis also increases. Necrosis develops very quickly.
Stages
First, an acute stage develops. In the absence of therapy, incomplete recovery is transformed into a chronic form. The final stage is ascites, often resulting in death.
- Activity in toxic hepatitis
Depending on It is determined by the dose, the presence of concomitant pathologies, speed, degree of activity. The most rapid rates of hepatitis develop with maximum toxic activity. Often it has a lethal outcome.
- Toxic hepatitis of minimal activity
The degree of activity is characteristic of toxic hepatitis. A favorable prognosis is hepatitis with a minimal degree of activity. It develops slowly, easily treatable. In general, its development is stimulated by a weakened immune system. This form is characterized by a mild inflammatory process that does not cause pain and does not cause discomfort to patients. It leads to an increase in size.
 [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37]
[27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37]
Forms
There are many varieties of hepatitis. In this regard, there are different classifications based on various factors. In accordance with the main classification, the disease is divided into acute and chronic. The acute process is characterized by a rapid progression of pathologies - due to the duration of the action of damaging factors. It develops slowly, it is less severe. The consequences and complications are no less serious.
There are many types of hepatitis. The most common are medicinal, professional, alimentary, viral, medicinal and alcoholic cirrhosis. Separately, toxic hepatitis is released with the transition to cirrhosis of the liver.
 [38], [39], [40], [41], [42], [43], [44], [45], [46]
[38], [39], [40], [41], [42], [43], [44], [45], [46]
Acute Toxic Hepatitis
A distinctive feature is that hepatitis is developing very rapidly, at a rapid pace. The peak of the disease occurs on the 3rd day of toxin exposure. There is intense pain that occurs as a result of hypertrophy. The temperature rises sharply, to 38 degrees and above. There is weakness, aches in the body, increased fragility, dyspeptic syndrome.
 [47], [48], [49], [50], [51], [52], [53], [54], [55], [56]
[47], [48], [49], [50], [51], [52], [53], [54], [55], [56]
Toxic medicinal hepatitis
Often toxicosis is a consequence of drug poisoning. The reason is excessive dosage or long-term use of medications. With prolonged admission, the chronic form most often develops, with an overdose - an acute form. The liver is often the only target organ that is exposed to toxins. The liver primarily reacts to the action of medicinal substances, since their processing takes place in the liver. Also, the liver neutralizes the remnants and introduces them to the outside.
Dosage and duration of drug intake varies widely. Currently, there are several thousand drugs that can cause liver damage. Often the cause of such complications is self-medication, since many such drugs are dispensed without a prescription. 50% fall on the mistakes of doctors who incorrectly prescribe drugs, or incorrectly combine them.
Some drugs have unavoidable side effects on the liver, regardless of the dose. But often, these medications can not be avoided. For example, chemotherapy, antiretroviral therapy, antitumor drugs. In people with increased sensitization of the body, frequent allergic reactions, in elderly people, the risk of developing toxic hepatitis increases with the intake of any medication. Even, at first glance, harmless antibiotics and antipyretics, can cause significant damage to the liver.
Especially dangerous for the liver are hormonal drugs, antidepressants, psychotropic substances and neuroleptics, diuretics, antibacterial and antiviral drugs. Some combinations of drugs may have toxic effects. Excess dosage of many drugs ends in a lethal outcome. So, if you take 10 g of paracetamol, liver necrosis develops. This drug is often taken with a suicidal purpose. Often toxic hepatitis develops after treatment of such diseases as leukopenia, splenomegaly.
The main condition for recovery is the withdrawal of drugs that have a toxic effect on the liver. It is also necessary to eliminate other causes that aggravate the inflammatory process. After this, appropriate therapy is conducted, which leads to the reverse development of pathology. If the measures are taken in a timely manner, the forecast can be favorable. In severe cases, hemodialysis, which usually has a positive effect, helps to restore the body. If liver failure develops, liver transplantation may be required urgently.
For the prevention of drug-induced hepatitis, the use of heavy drugs that have side effects must be combined with hepatoprotectors. They protect against negative effects, reduce the likelihood of damage and the severity of the pathology.
Alcoholic Toxic Hepatitis
Alcohol, especially substandard, has a negative effect. It is neutralized in the liver. There are toxins that have a damaging effect in man. They are necrosis, which ultimately contributes to cirrhosis, lethal outcome.
Occupational Toxic Hepatitis
It is a consequence of the impact on the body of harmful production factors. Most often observed in employees who have worked for a long time in the field of production, in laboratories. Especially the risk of occupational hepatitis in employees with reduced immunity and concomitant viral hepatitis, or other liver diseases is increased.
It can develop in both acute and chronic forms. In acute form develops as a result of industrial leaks, through negligence, in case of equipment malfunction or idle exhaust. In this case, the body immediately receives a large dose of the drug.
In chronic form, poisoning develops slowly, gradually. For example, a person inhales for a long time a pair of poisonous substances. The main industrial poisons are yellow phosphorus, trichlorethylene, carbon. Biological agents, for example, fungi, viruses, bacteria, with which microbiologists, virologists, and bacteriologists have to work are also dangerous. No less dangerous are pharmaceutical and chemical products that are used for medicinal purposes or for research.
Alimentary toxic hepatitis
This form of the disease is also called fecal-oral hepatitis. The main cause of the disease are fragments of fecal matter, which come from an infected person to a healthy one. Distribution occurs through the mouth, with oral contact. Exposed to this form of infection are people with a craving for unconventional methods of sexual relations.
Such a mechanism erroneously suggests that toxic hepatitis is contagious. But this is not so. It must be understood that not the disease itself is transmitted, but the toxic agent that causes it. It is he who leads to the development of similar damage in the body.
 [59], [60], [61], [62], [63], [64], [65]
[59], [60], [61], [62], [63], [64], [65]
Viral Toxic Hepatitis
The cause of the development is the virus, which secretes into the blood toxins and products of viral metabolism. These substances are called endotoxins. They penetrate the liver and have pathological changes in it, including necrosis and fatty degeneration of the liver. Viral hepatitis is confirmed by virological studies. Sometimes the disease is hidden, therefore it is important to undergo a preventive examination, take tests. This will allow timely detection of pathology and take the necessary measures.
Treatment depends on which form of the virus caused the change. This can not do without laboratory tests. Viral hepatitis B, C, D are transmitted sexually and with addiction. Also, infection can occur during surgical interventions, with invasive procedures as a result of non-compliance with asepsis rules.
The most severe is hepatitis C. Externally, the disease can not always be manifested. A person can feel quite well, after which there is a sharp crisis. The liver is damaged slowly and asymptomatically. It manifests itself in the end with cirrhosis of the liver, after which a person quickly dies. In addition, he can give complications to other organs.
Hepatitis B is widely distributed among the population and is often transmitted through blood transfusion. The main preventive measure is the control of donor blood and regular preventive examination. If detected in time, is treatable. But with late detection often ends in a lethal outcome.
Hepatitis D is often layered on hepatitis B. Together they form a dangerous disease that manifests itself in severe form and gives serious complications. In most cases it ends lethal.
Toxic hepatitis after chemotherapy
One of the leading causes is the impact of chemotherapy and antiviral therapy, one hundred contributes to liver damage in both acute and chronic forms. This is due to the fact that the main cleavage of antitumor drugs occurs in the liver. As a result, all liver functions, including detoxification, are violated. Cytostatics stop the growth and division of tumor cells, but at the same time, they have a similar effect on liver cells. Cells lose the ability to regenerate. This leads to the fact that the drug accumulates in the liver and has a toxic effect on the liver. As a result of chemotherapy, toxic hepatitis is complicated by cholestatic impairment of hepatic encephalopathy. All this is accompanied by a rash, pain. The body temperature rises substantially.
In order to minimize the negative effect of chemotherapy on the liver, it is necessary to carry out constant liver monitoring. The main analysis is a biochemical blood test. In accordance with modern requirements, the blood test must be taken before the start of chemotherapy, and then on the 14th day of treatment. The state from 14 to 21 days is carefully monitored. At this time, often tests are taken daily. Trace the indicators of bilirubin and transaminases, which are a sign of toxic damage to the liver. After the end of cancer therapy, the liver is monitored for 6 months on a monthly basis, then every 6 months.
To prevent toxicosis during chemotherapy is possible by carrying out hepatoprotection. It restores the structure of damaged membranes, inhibits destructive processes in hepatocytes, prevents fibrosis.
Exogenously toxic hepatitis
Caused by exposure to external toxins. These are elements of any nature and origin, including heavy metals, acid pairs, alcohol, medicines. Can provoke both acute and chronic form of the disease. At the heart of the pathogenesis is mainly the violation of hemostasis of the liver.
Often, exogenous poisoning occurs in agriculture when treated with insecticides, herbicides. The most severe forms are observed when poisoning with arsenic, carbon, phosphorus. Many medications, and even hormonal contraceptives, damage the liver.
Complications and consequences
Toxic hepatitis rarely passes without consequences. The exception is when it occurs in a mild form and is detected in the early stages. Then it is possible to conduct a timely treatment and cure the disease. Otherwise, numerous pathologies develop, including hepatic insufficiency, coma. Liver failure - hepatocytes are replaced by fat cells. This manifests itself in the form of edema. Clotting decreases substantially, its properties change. The person sharply grows thin, because he does not have enough fats, which are produced by the liver. Also there is not enough energy, which is accompanied by weakness and increased fatigue. Hepatic encephalopathy also develops. The process is constantly progressing, cramps appear. Can end fatal. The final stage can be cirrhosis of the liver. When the cells are completely killed and replaced. Leads to death.
Toxic hepatitis with outcome in cirrhosis
The most serious complication. There are three stages of development: compensatory, subcompensation and decompensational. First, the disease goes into a compensatory stage, which manifests itself as a mild inflammatory process, tissue damage, scarring begins. Functional activity is sharply reduced, but at this stage the body can still compensate for lost functions.
When the transition to the subcompensation stage, symptoms of liver damage appear, the connective tissue grows significantly.
The third stage - decompensational, is the most dangerous. Often ends with a fatal outcome. At this stage, scar tissue takes up most of the liver. There is a huge risk of developing liver failure and coma. Often these conditions end in death.
 [73], [74], [75], [76], [77], [78], [79]
[73], [74], [75], [76], [77], [78], [79]
Ascites in Toxic Hepatitis
Ascites is a pathological condition in which fluid accumulates in the abdominal cavity. This is due to a pathological exchange, as a result of which the normal outlet of the liquid is disturbed. There is a squeezing of the internal organs, there are accompanying pathologies, gastroenterological pathologies.
Ascites can develop slowly. The heaviest degree squeezes the diaphragm, breathing is broken. After the appearance of ascites, the disease passes into the terminal stage.
If there is severe bleeding and collapse - often indicates a portal vein rupture, which could not stand the pressure.
Diagnostics of the toxic hepatitis
Various methods are used to make the diagnosis. They make an examination, collect an anamnesis of the patient's life. Based on these data, the necessary laboratory and instrumental studies are assigned. Differential diagnostics with other diseases, which have similar signs, is carried out. After this, an accurate diagnosis is made.
The rationale for the diagnosis of toxic hepatitis
For the correct selection of treatment is not enough to just make a diagnosis, you still need to justify it. To do this, it must be confirmed that it is of a toxic nature. Most often a toxicological study is conducted, which determines which substance caused damage in the liver. After this, the most important condition for successful treatment is the termination of this factor on the body. If the substance continues to have toxic effects, recovery is impossible, even with complex therapy.
Laboratory indicators for toxic hepatitis
On the development of hepatitis indicates an increase in the level of bilirubin up to 800-850 μmol / l. When considering bilirubin by fractions, you can notice that the predominant is direct bilirubin, its values are about 1.5 times higher than the amount of indirect bilirubin.
The study of urine shows positive results when carrying out the reaction with bile pigments and urobilin. There is moderate proteinuria. Bilirubin in toxic hepatitis
The liver damage of various etiologies is indicated by an increase in bilirubin in excess of 17.1 μmol / l. The indicator is up to 86 μmol / l for an easy form of hepatitis, on average - up to 159. Heavy form can be spoken at a level above 160 μmol / l.
Instrumental diagnosis of liver and spleen are normal. If these data are insufficient to make an accurate diagnosis, computer and magnetic resonance imaging (CT and MRI), liver scintigraphy, are used.
By scintigraphy is meant a new method of diagnosis, in which radioactive isotopes are introduced into the human body. The substances are injected through the vein. After 15 minutes, begin the study. The resulting radiation makes it possible to visualize the image of internal organs and display it on the screen. This method determines the functional characteristics of the organ and determine the size of the liver. The duration of the procedure is approximately 20 minutes.
Biopsy or laparoscopy with targeted biopsy may be necessary.
What do need to examine?
Differential diagnosis
The essence of differential diagnosis is to accurately separate toxic hepatitis from another disease that has similar manifestations. After the diagnosis is confirmed - hepatitis, further differentiation is carried out, the purpose of which is to determine its type. In this case it is necessary to confirm that we are dealing with toxic hepatitis, which is caused by the action of toxic substances on the body.
For this, various diagnostic methods are used. To confirm hepatitis most often apply instrumental diagnostic methods, laboratory studies. Hepatitis can be indicated by splenomegaly, leukopenia, elevated bilirubin level. When performing ultrasound, a peculiar clinical picture is characteristic of hepatitis.
In order to establish the nature of the damaging factor, serological analyzes are conducted. Toxicological analysis may indicate an increased level of toxin in the blood. Virological and serological studies will show the absence of viral load in the body, which will exclude hepatitis of viral etiology. If you suspect a hepatitis of alcoholic etiology, you may need to consult a toxicologist, an expert in narcology. Also, an immunological study is carried out for the presence of antibodies in the blood that are characteristic of autoimmune hepatitis.
 [90], [91], [92], [93], [94], [95], [96]
[90], [91], [92], [93], [94], [95], [96]
Differential diagnosis of viral hepatitis with toxic hepatitis
To differentiate toxic hepatitis from viral, it is possible on the basis of the results of toxicological and virological (serological) studies. With viral hepatitis, an increased concentration of antibodies to the hepatitis virus is detected, or the viruses themselves are detected. It all depends on the method of diagnosis. This is a direct confirmation or refutation of the diagnosis. To confirm the toxic nature of hepatitis, toxicological diagnostics is carried out. Detect the amount of toxin and its appearance.
Who to contact?
Treatment of the toxic hepatitis
There are many different treatments for toxic hepatitis. But they are based on standard principles, which must be observed. Any successful therapy should be based solely on these principles.
More information of the treatment
Prevention
Prevention is reduced to careful monitoring of food intake. If in the workplace a person works with harmful factors, it is necessary to strictly observe the rules of safety and personal hygiene. The room should be ventilated, work should be done under the hood. When taking medications, you should strictly follow the dosage, follow the doctor's recommendations. If necessary, additionally take hepatoprotectors. You need to give up alcohol, or take exceptionally high-quality alcohol. When the first signs of the disease appear, you need to see a doctor as soon as possible.
Forecast
It all depends on the severity of the disease and on how quickly the right treatment was prescribed. With an easy stage of the disease, the prognosis may be favorable. The liver can be fully restored if the disease is diagnosed in time and treatment is started. Complete recovery is possible with further regular passage of preventive examinations and maintenance therapy.
If the disease becomes chronic or severe, the risk of complications increases. Hepatocyte damage progresses. The cells gradually die off and are replaced by a connective tissue. The most dangerous complications of severe hepatitis are hepatic insufficiency, coma and cirrhosis of the liver. At the same time, the prognosis can be extremely unfavorable, up to a lethal outcome. At occurrence of an ascites it is necessary to expect fast death. As a rule, patients with ascites die within a few days and only 10% manage to survive with such pathology a month.
How many live with toxic hepatitis?
With the diagnosis of toxic hepatitis, the duration and quality of life largely depend on the patient himself. It is necessary to conduct complete and timely treatment, fully comply with the doctor's recommendations, and also follow the diet and bed rest. In this case, the person will recover quickly enough. But in the future he will need regular preventive examinations and maintenance therapy. In this case, you can live for decades. If you ignore the diagnosis and treatment, the disease can go to cirrhosis and ascites, which ends in a fatal outcome. With such complications, people live from a few months to two years.

