Medical expert of the article
New publications
Staphylococcus in a swab of throat, nose: causes, treatment
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Staphylococci are one of the most common groups of microorganisms that combine saprophytes and pathogens of human and animal diseases. Despite the relative simplicity of detection of staphylococci in biological material from patients and environmental objects, in practice there are numerous difficulties. This is due to the fact that staphylococci are representatives of normal microflora, because staphylococcus in the smear is not always an objective evidence of their aetiological role in the development of the disease. It is also necessary to take into account the diversity of their manifestations, the degree of pathogenicity, the wide variability under the action of antibacterial agents, the extraordinary variety of clinical forms.
That is why the scheme of diagnosis and treatment of this infection can not be universal, but should be developed taking into account the specific specific nosological form of the disease. In addition, an important measure is the combined determination of qualitative and quantitative indices of the content of pathogenic staphylococci in the material under study.
Foodborne toxicinfection of staphylococcal etiology in number of cases occupy one of the leading places among poisonings of bacterial nature.
The norm of staphylococcus in the smear
Normally, staphylococcus must be present in the smear, because it is a representative of normal microflora. Its absence or low index also has a negative impact on health, as well as overestimated indicators. As a rule, the indicator is considered to be up to 103 (10 in 3). Any deviation is considered a violation, either in the direction of increasing the concentration or in the direction of its decrease. An increase above this indicator is a pathological condition in which the release of staphylococcus into the environment occurs, even with quiet breathing.
Staphylococcus in smear 10 in 3 - 10 in 5
The unit of measurement during the quantitative analysis is CFU / ml - the number of colony forming units in 1 ml of the biological material being studied.
To perform calculations and determine the degree of contamination, first count the number of homogeneous colonies that have grown in the Petri dish after sowing. They should be identical in color and pigmentation. Then recalculate from the number of colonies to the degree of seeding.
Let's consider on a concrete example. For example, if the cup has grown 20 CFU, this means that in 0.1 ml of the test material contained 20 colonies of microorganisms. Calculate the total amount of microorganism can be as follows: 20 x 10 x 5 = 1000, or 103 (10 in 3). In this case, proceed from the fact that 20 is the number of colonies that grew on a petri dish, 10 is the number of colony forming units in 1 ml, given that only one tenth of the microorganisms were sown, 5 is the volume of physiological solution in which it was diluted try.
The concentration of 104, (10 in 4) is determined in the same way, which many specialists consider as a boundary condition between the relative norm and a pronounced pathology, at which bacteremia and acute inflammatory process develops. As an absolute pathology the indicator 105 (10 in 5) is considered.
Causes of the staphylococci in the smear
Staphylococcus within the norm will always be found in the smear, because it is a representative of normal microflora. Therefore, from the point of view of bacteriology, it makes sense to discuss the reasons for the increase in the quantitative indicators of staphylococcus aureus. Thus, the concentration of staphylococcus increases in the first place with reduced immunity. Normally, the immune system produces protective factors (histocompatibility complex, interferons, immunoglobulins others) that stimulate the normal state of the mucous membranes, prevent uncontrolled reproduction of the bacterial flora, and suppress active growth.
Another reason is dysbiosis. Due to various reasons, the number of representatives of normal microflora is reduced. As a result, "free space" appears, which is immediately occupied by other microorganisms, including staphylococcus aureus. It is one of the first microorganisms that colonize free space, and reliably attach to it. As a result, the quantitative indicators increase sharply.
The causes of dysbacteriosis are many. Perhaps the most important is the intake of antibiotics, since there are practically no antibiotics directed solely on the causative agent of the disease. All of them are preparations with a wide spectrum of action. They affect not only the specific pathogen, but also the accompanying flora. Chemotherapy, antitumor treatment is similarly affected.
Reducing the immunity and disruption of normal microflora contributes to hypothermia, overfatigue, constant nervous and mental overstrain, stress, non-compliance with the regime of the day. Negatively reflected inadequate and inadequate nutrition, lack of vitamins, trace elements, bad habits, unfavorable living conditions and work.
Staphylococcus in a swab of throat
A smear from the throat is taken during preventive research for workers in the field of catering and child care, as well as for the diagnosis of infectious diseases (only if there are indications). The main indication is the presence of inflammatory processes in the nasopharynx, pharynx.
The development of staphylococcal infection, food poisoning originates precisely from the oral cavity and throat. Often, the microorganism persists in the area of throat, nasopharynx, and the person does not even know about it, because in the early stages the pathological process can be asymptomatic. Nevertheless, its amount increases, which can subsequently lead to chronic pathology, acute inflammation, sore throat, enlarged lymph nodes. In addition, with increased concentration of the microorganism, it is released into the environment. As a result, a person becomes a carrier. In this case, the person himself can not get sick, but he infects the surrounding people.
When detecting staphylococcus in a smear from the throat, people are not allowed to work at food enterprises, culinary workshops, canteens, which helps to avoid food intoxication. Also, bacterial carriers are not allowed to work with children, especially for children of early, preschool, younger age. Required sanitation is underway
Identification of the exact concentration of staphylococcus in the smear makes it possible to accurately identify the pathogen and diagnose the pathological process, to select the optimal treatment.
The sampling of the material for the study is done with a sterile tampon, by carrying them along the surface of the tonsils. Be sure to take the material taken on an empty stomach, or not earlier than 2-3 hours after eating. It is compulsory to take the material before antibiotic therapy, otherwise the results will be distorted.
Then, under laboratory conditions, the plant material is sown to nutrient media. Sow the material in the next 2 hours after the fence. The optimal medium for sowing staphylococcus is milk-salt agar, yolk agar.
 [1], [2], [3], [4], [5], [6], [7]
[1], [2], [3], [4], [5], [6], [7]
Staphylococcus in a smear from the nose
A smear from the nose is taken in the study of certain categories of workers (work with children, in the field of public catering). The fence is made with a sterile swab from the nasal mucosa. At the same time, each nostril uses its own, a separate tampon. In this case, the nasal cavity should not be treated in any way, the rinsing should not be carried out the day before. The fence is made before antibiotic therapy, otherwise the result will be invalid.
The analysis is done on average 5-7 days. After sampling the material, it is sown directly on the surface of the nutrient medium. For seeding, 0.1 ml of flushing is used. It is convenient to use Baird-Parker medium, on which it is very easy to recognize colonies of staphylococcus by opalescent gloss, black colonies. In general, the choice of the environment is determined by the laboratory assistant, depending on the provision of the laboratory and individual research objectives, specialization and qualification level. The ratio of seed to nutrient medium is 1:10. Then incubate under thermostat conditions.
Then, on day 2-3, carried out by reseeding on sloping agar, a pure culture is allocated. With it, further studies are carried out (biochemical, immunological), the main properties are determined, the culture is identified, the concentration is determined, if necessary, sensitivity to antibiotics.
Separately, microscopy is performed, which makes it possible to determine an approximate preliminary assessment of the smear, to reveal the specific accessory of the microorganism according to the characteristic morphological and anatomical features. It is also possible to detect other signs of pathology: signs of inflammation, neoplasms.
A person is given only a ready result, indicating the type of microorganism, the degree of dissemination, and sometimes the sensitivity to antibacterial drugs.
Staphylococcus in a vaginal smear
Detect, because they are permanent inhabitants of the skin and mucous membranes. The diseases that cause staphylococcus are of an autoinfection nature, that is, they develop when the basic parameters of the biochemical cycle of a person change, the hormonal background changes, microflora, damage to the mucous membranes, pregnancy. Less often result from exogenous infection (from the external environment).
Staphylococcus in the swab of the cervical canal
Can be detected against a background of dysbiosis, which develops during pregnancy, a decrease in microflora, a violation of the hormonal cycle. Since staphylococcus is characterized by a wide range of sources of infection and polyorganism, they can easily be transported with blood and cause inflammation outside the main source. Often the development of staphylococcal infection is a consequence of antibiotic therapy, physiotherapy, and surgical interventions.
Risk factors
People with a pathological focus of infection in the body are at risk. For example, staphylococcal infection can develop in the presence of caries in the oral cavity, inflammation of the tonsils, chronic and not fully cured respiratory tract diseases, urogenital organs, in the presence of purulent-septic wounds, burns, skin and mucous membranes. Catheters, implants, transplants, prostheses are of great danger, as they can be colonized by staphylococcal infection.
Risk factor is reduced immunity, disruption of the endocrine system, dysbiosis, gastrointestinal tract diseases. People who have recently undergone surgical intervention, after serious illnesses, after antibiotic therapy, and chemotherapy also fall into the risk group.
A separate group consists of people with immunodeficiencies, AIDS, other infectious diseases, autoimmune pathologies. Newborn children are at risk (due to the unformed microflora and immune system), pregnant women (on the background of hormonal rearrangements). The mothers and puerperas, because at present hospitals and maternity hospitals are seriously endangered with nosocomial strains of staphylococcus that live in the environment, they have acquired multiple resistance and increased pathogenicity. They are easy enough to get infected.
The risk group includes people who do not observe the regime of the day, do not eat enough, are exposed to nervous and physical stress and overstrain.
A special group is represented by medical personnel, biologists, researchers who work with different cultures of microorganisms, including staphylococcus, have contact with biological fluids, tissue samples, feces, are in constant contact with both infectious and non-infectious patients.
Here, too, include laboratory assistants, nurses, nurses, employees of sanitary authorities, pharmacists, developers of vaccines and toxoids, and their testers. Also, agricultural workers who deal with animals, livestock and poultry products, which are also a source of infection, are at risk.
Symptoms of the staphylococci in the smear
Symptoms directly depend on the localization of the focus of infection. Thus, with the development of an infection of the respiratory tract, first colonization of the mucosa of the oral cavity and the nasopharynx takes place. This manifests itself in the form of inflammation, swelling, and hyperemia. There is pain when swallowing, perspiration, burning in the throat, stuffy nose, joins a rhinitis with the allocation of yellow-green mucus, depending on the severity of the pathology.
As the infectious process progresses, signs of intoxication develop, the temperature rises, weakness appears, the general resistance of the organism decreases, immunity decreases, resulting in the pathological process only aggravated.
There may be signs of systemic organ damage. On the descending airways, the infection descends downward, causing bronchitis, pneumonia, pleurisy with a strong cough, plentiful separation of sputum.
With the development of infection in the genitourinary tract and reproductive organs, irritation of mucous membranes first develops, itching, burning, and hyperemia occur. Gradually, the pathological process progresses, inflammation, pain, white discharge with a specific odor. There is pain when urinating, burning. Progression of the disease leads to the development of an intensive infectious process, which extends to the area of the rectum, perineum, internal organs.
With the localization of the inflammatory process on the skin and the wound surface, the wound is wounded, there is a specific smell, local and then the body temperature may increase. The foci of infection spreads all the time, the wound "wets", does not heal, it grows all the time.
With the development of staphylococcal infection in the intestinal tract, there are signs of food poisoning: nausea, vomiting, diarrhea, indigestion, stools, decreased appetite. There is pain and inflammation in the gastrointestinal tract: gastritis, enteritis, enterocolitis, proctitis. When generalizing the inflammatory process and increasing signs of intoxication, the body temperature rises, chills, fever develops.
First signs
Early symptoms are known, which are harbingers of the disease. They develop as the concentration of staphylococcus in the blood increases, and appear long before the real symptoms appear.
So, the development of staphylococcal infection is accompanied by increased heart rate and respiration, there is a shiver in the body, chills, fever. When walking, increased strain, there may be a strain on the heart, lungs, there is a slight shortness of breath. There may be headache, migraine, stuffiness of the nose, ears, less often - tearing, perspiration and dryness in the throat, dry skin and mucous membranes.
Often there is a feeling of elevated temperature, but when measured, it remains normal. The person quickly becomes tired, working capacity sharply decreases, there is an irritation, tearfulness, drowsiness. The concentration of concentration, the ability to concentrate, can decrease.
Staphylococcus aureus in smear
Staphylococcus aureus, S. Aureus, is a frequent causative agent of inflammatory and infectious diseases of the internal organs of man and animals. There are more than 100 nosological forms of diseases caused by this pathogen. At the heart of the pathogenesis of Staphylococcus aureus lies a whole complex of toxic substances and factors of aggression, enzymes that are produced by microorganisms. In addition, it was found that the pathogenicity of the microorganism is due to genetic factors and the influence of the environment.
It is worth emphasizing that Staphylococcus aureus has polyorganic tropism, that is, it can become the causative agent of the pathological process in any organ. This manifests itself in the ability to cause purulent-inflammatory processes in the skin, subcutaneous tissue, lymph nodes, respiratory tract, urinary system, and even the musculoskeletal system. It is a frequent causative agent of food poisoning. The special significance of this microorganism is determined by its role in the etiology of nosocomial infections. Among Staphylococcus aureus often there are methicillin-resistant strains that are highly resistant to the action of any antibiotics and antiseptic agents.
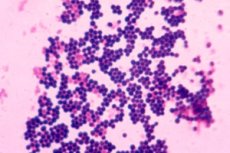
In the smear it is easy enough to recognize, since it has the form of gram-positive cocci, whose diameter varies from 0.5 to 1.5 μm, are arranged in pairs, in short chains or clusters in the form of a cluster of grapes. Fixed, do not form a dispute. Grow in the presence of 10% sodium chloride. Surface structures are capable of synthesizing a number of toxins and enzymes that play an important role in the metabolism of microorganisms and determine their role in the etiology of staphylococcal infections.
Also in the smear it is easy to recognize by such morphological features as the presence of the cell wall, membrane structures, capsule and flocculating factor. An important role in pathogenesis is played by the aglutinogen A protein, which is evenly distributed throughout the thickness of the cell wall and is covalently linked to peptidoglycan. The biological activity of this protein is diverse and is an unfavorable factor for the macroorganism. It is able to react with mucosal immunoglobulin, form complexes that are accompanied by damage to platelets and the development of thromboembolic reactions. It is also an obstacle to active phagocytosis, contributes to the development of an allergic reaction.
Epidermal staphylococcus in the smear
For a long time it was believed that epidermal staphylococcus does not have pathogenicity. But recent studies have confirmed that this is not so. Is a representative of the normal microflora of skin and can cause disease in some people. Especially it concerns people with reduced immunity, after burns, damage to the integrity of the skin, with various injuries. As a result of the development of staphylococcal infection, a purulent-septic inflammatory process develops quite quickly, zones of necrosis, erosion, ulcers, suppuration appear.
In the smear it is easy enough to recognize the formation of pigmented colonies, with a diameter of up to 5 mm. Form a form of cocci, can be single or combine in polycompounds, reminiscent of grapes. They can grow both in aerobic and anaerobic conditions.
Hemolytic staphylococcus in smear
Hemolytic properties of staphylococcus is its ability to lysed blood. This property is ensured by the synthesis of plasmacoagulase and leukocidin, bacterial toxins that break down blood. It is the ability to split and coagulate plasma, is the leading and constant criterion by which pathogenic staphylococci are easily identifiable.
The principle of the reaction is that the plasmacoagulase reacts with the Co-factor of the plasma, forms coagulazotrombin with it, which converts thrombinogen to thrombin to form a blood clot.
Plasmacoagulase is an enzyme that breaks down quite easily under the action of proteolytic enzymes, for example, trypsin, chemotripsin, and also when heated to a temperature of 100 degrees and higher for 60 minutes. Large concentrations of coagulase lead to a decrease in the ability of the blood to clot, hemodynamics is disturbed, oxygenation of tissues occurs. In addition, the enzyme promotes the formation of fibrin barriers around the microbial cell, thereby reducing the effectiveness of phagocytosis.
Currently, 5 types of hemolysins are known, each of which has its own mechanism of action. Alpha toxin is not active against human erythrocytes, but lysates erythrocytes of sheep, rabbits, pigs, aggregates platelets, has a lethal and dermonecrotic effect.
Beta-toxin causes lysis of human erythrocytes, has a cytotoxic effect on human fibroblasts.
Gamma toxin lyses human erythrocytes. Its lytic action on leukocytes is also known. Does not have a toxic effect when administered intradermally. When intravenously leads to death.
Delta-toxin differs from all other toxins by its thermolability, a wide spectrum of cytotoxic activity, damages erythrocytes, leukocytes, lysosomes and mitochondria.
Epsilon-toxin provides the widest possible area of action, lysing all types of blood cells.
Coagulase-negative staphylococcus in smear
The importance of coagulase-negative staphylococci in the development of pathology of internal organs is beyond doubt. As the researchers believe, this group is responsible for the development of the pathology of the urogenital tract in about 13-14% of cases. They are the causative agents of skin and wound infections, conjunctivitis, inflammatory processes and sepsis in newborns. The most severe form of infection is endocarditis. Especially the number of such complications increased due to the high prevalence of heart operations when installing artificial valves and shunting blood vessels.
Considering biological properties, it is worth noting that microorganisms are cocci with a diameter of no more than 5 microns, pigments do not form, can grow both in aerobic and anaerobic conditions. Grow in the presence of 10% sodium chloride. Capable of haemolysis, nitrate reduction, urease, no DNA production. Under aerobic conditions, they are able to produce lactose, sucrose, mannose. Not capable of fermenting mannitol and trehalose.
The most important is epidermal staphylococcus, which is one of the leading clinically significant pathogens. It causes septicemia, conjunctivitis, pyoderma, urinary tract infections. Also among coagulase-negative strains there are many representatives of nosocomial infections.
Staphylococcus saprophyticus, saprophytic in the smear
Refers to coagulase-negative strains that are able to exist, both in aerobic and anaerobic conditions. Actively multiply in the wound surface, in damaged areas of the skin, with severe burns, with a foreign body in soft tissues, with grafts, prostheses, with invasive procedures.
Often lead to the development of toxic shock. This effect is due to the action of endotoxins. It often develops using sorbing tampons in women during menstruation, in the postpartum period, after abortion, miscarriages, gynecological operations, after prolonged use of barrier contraception.
The clinical picture is represented by a sharp rise in temperature, nausea, sharp pains in the muscles and joints. Later, typical spotted rashes appear, most often generalized. Develops arterial hypotension, accompanied by loss of consciousness. Mortality reaches 25%.
Staphylococcus aureus in a smear
It is the main causative agent of food toxic infections. Well preserved in the environment. The main route of transmission is fecal-oral. It is released into the environment with feces. It enters the body with poorly digested food, dirty hands, unwashed products.
The mechanism of action is due to staphylococcal enterotoxins, which are thermostable polypeptides formed during the multiplication of enterotoxigenic strains, staphylococci in food, intestines and artificial nutrient media. They show high resistance to the action of food enzymes.
The enteropathogenicity of toxins is determined by their association with the epithelial cells of the stomach and intestine, by affecting the enzymatic systems of epithelial cells. This, in turn, leads to an increase in the rate of formation of prostaglandins, histamine, increased secretion of fluids in the lumen of the stomach and intestines. In addition, toxins damage membranes of epithelial cells, increasing the permeability of the intestinal wall to other toxic products of bacterial origin.
The virulence of fecal enteropathogenic staphylococci is regulated by the genetic apparatus of the bacterial cell in response to the action of environmental factors, which allows the microorganism to quickly adapt to environmental conditions, which allows the microorganism to quickly adapt to changing conditions in the transition from one microbiocenosis to another.
Differential diagnosis
In determining the role and significance of various members of the genus Staphylococcus in the etiology of purulent-inflammatory diseases of man, despite the relative simplicity of their detection, are associated with numerous difficulties. This is due to the fact that staphylococcus is a representative of normal microflora, which inhabits various biotopes of the human body. It is necessary to clearly distinguish endogenous staphylococcus, which develops inside the body, as well as endogenous, which penetrates into the body and the environment. It is also important to understand which of the biotopes of the human body is typical for him, and where he is the representative of the transient flora (recorded accidentally).
It is also important to take into account the high variability of the microorganism under the influence of various factors, including antibiotics. A wide variety of clinical manifestations and nosological forms are taken into account. Therefore, the universal scheme for diagnosis of staphylococcal infection. It is easier to study those biological environments that are normally sterile (blood, urine, liquor). In this case, the detection of any microorganism, the colony is a pathology. The most difficult is the diagnosis of diseases of the nose, pharynx, intestine, a study on bacterial transport.
In the most general form, the diagnostic scheme can be reduced to the correct collection of biological material, carrying out its bacteriological primary seeding on an artificial nutrient medium. At this stage, preliminary microscopy can be carried out. By studying the morphological, cytological features of the sample, it is possible to obtain certain information about the microorganism, to conduct at least its generic identification.
To obtain more detailed information, it is necessary to select a pure culture and conduct further biochemical, serological and immunological studies with it. This allows us to determine not only the generic, but also the species affiliation, as well as determine the biological belonging, in particular, the serotype, biotype, phagotype and other properties.
Who to contact?
Treatment of the staphylococci in the smear
Staphylococcal infection requires antibiotic therapy. Therapy is exclusively etiological, that is, it is aimed at eliminating the cause of the disease (actually the bacteria), or, more precisely, reducing its degree of dissemination to normal levels. Various antibiotics are used.
Some doctors prefer to use a wide range of drugs, while others prescribe antibiotics to their patients, aimed exclusively at eliminating gram-positive infections, including staphylococcus aureus. The choice is mainly determined by the results of antibiotic susceptibility testing, as a result of which the most effective drug is determined and its optimal dosage is selected.
In some, mild cases for correcting the condition, antibiotic therapy may not be needed. It may just require the normalization of microflora. This is observed with dysbiosis. In this case, prescribing probiotics, prebiotics, which normalize the state of microflora by reducing the amount of pathogenic flora and increasing the concentration of representatives of normal microflora.
Symptomatic therapy is rarely used, as it is usually enough to eliminate the infection, and the attendant symptoms will disappear on their own. In some cases, additional measures are prescribed, for example: analgesics, anti-inflammatory, antihistamines, antiallergic agents. When skin diseases are used external means: ointments, cream. Physiotherapy, folk and homeopathic remedies can be prescribed.
Vitaminotherapy is not carried out, since vitamins act as growth factors for microorganisms. The exception is vitamin C, which must be taken at a dosage of 1000 mg / day (double dose). This will increase the immunity, resistance, and resistance of the body to adverse factors.
Medications
The treatment of infectious diseases should be approached seriously. Self-medication can not be dealt with, often it has deplorable consequences. It is necessary to take into account a lot of nuances before starting treatment. Only the doctor can do this best.
It is important to observe precautions: do not treat the infection "blindly", even with a pronounced clinical picture. It is necessary to carry out a bacteriological study, isolate the causative agent of the disease, select the most optimal antibiotic directly to it, determine the necessary dosage, which will completely suppress the growth of the microorganism.
It is also important to undergo a complete course, even if the symptoms have disappeared. This is due to the fact that if you quit treatment, the microorganisms will not be completely killed. Surviving microorganisms will quickly become resistant to the drug. When re-applied, it will be ineffective. Moreover, resistance to the entire group of drugs, and to similar drugs will be developed (due to the development of a cross reaction).
Another important precautionary measure is that you yourself can not reduce or increase dosage on your own. Reduction may not be effective: the bacteria will not be killed. Accordingly, they mutate in a short time, they will acquire stability and a higher degree of pathogenicity.
Some antibiotics can also have side effects. The stomach and intestines are especially sensitive to antibiotics. It can develop gastritis, dyspeptic disorders, stool, nausea. Some have a negative effect on the liver, so they need to be taken together with hepatoprotectors.
Below are the antibiotics, which are well established in the treatment of staphylococcal infection with minimal side effects.
Amoxiclav is effective in the treatment of staphylococcal infection of any location. It is used in the treatment of diseases of the respiratory tract, urogenital system, intestines. Take 500 mg per day for three days. If necessary, repeat the treatment.
Ampicillin is prescribed primarily for diseases of the upper and lower respiratory tract. The optimal dosage is 50 mg / kg body weight.
Oxacillin is effective both in local inflammatory processes and in generalized infection. Is a reliable prophylaxis of sepsis. Assigned to 2 grams every 4 chavs. Enter intravenously.
When purulent-inflammatory skin diseases externally apply levomitsetinovuyu ointment, applying it a thin layer on the damaged surface. Also inside take Levomycetin 1 gram three times a day. With a strong generalization of the infectious process, Levomycetin is administered intramuscularly, 1 gram every 4-6 hours.
Candles from Staphylococcus aureus
Applied mainly with gynecological diseases, infections of the urinary tract, less often - with intestinal dysbiosis with inflammation of the rectum. Prescribe candles and choose the optimal dosage can only the doctor, because with improper application, the risk of complications and further spread of infection is high. Candles are not prescribed without preliminary analysis. Indication for their use is exclusively staphylococcus in the smear.

