
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Examination of the respiratory function of the nose
Medical expert of the article
Last reviewed: 07.07.2025
A person suffering from nasal breathing problems can be identified at first glance. If this deficiency has accompanied him since early childhood (chronic adenoiditis), then signs of nasal respiratory failure are detected during a quick examination of the face: a slightly open mouth, an abnormally developed skeleton of the facial part of the skull ( prognathism and underdevelopment of the lower jaw), abnormal development of teeth and the nasal pyramid, smoothing of the nasolabial folds, closed nasality (difficulty pronouncing the sonorant sounds "an", "en", "on", etc.) - due to a violation of the resonator function of the nose. Vauquez syndrome may also be observed, which occurs with juvenile deforming recurrent nasal polyposis, manifested by clear signs of obstruction of the nasal passages, thickening and widening of the nasal bridge. These signs of nasal breathing disorders are confirmed by its objective causes, revealed during anterior and posterior (indirect) rhinoscopy or with the help of modern rhinoscopes equipped with special optics. As a rule, "physical" obstacles are detected in the nasal cavity or in the nasopharynx area, disrupting the normal functioning of the nasal aerodynamic system (polyps, hypertrophied nasal conchae, curvature of the nasal septum, tumors, etc.).
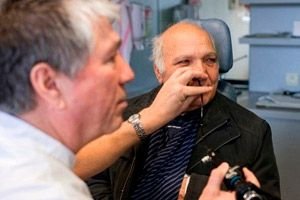
There are many simple ways to assess the state of nasal breathing, allowing to obtain the necessary data without resorting to complex and expensive methods, such as computer rhinomanometry. For example, the patient breathes only through the nose, the doctor observes him. When nasal breathing is difficult, the frequency and depth of breathing changes, characteristic noises appear in the nose, movements of the wings of the nose are observed, synchronizing with the phases of breathing; with a sharp difficulty in nasal breathing, the patient switches to the mouth type of breathing with characteristic signs of dyspnea in a few seconds.
Impaired nasal breathing of each half of the nose can be determined by very simple methods: by placing a small mirror, a forehead reflector or the handle of a metal spatula to the nostrils (the degree of fogging of the surface of an object brought to the nose is assessed). The principle of studying the respiratory function of the nose by determining the size of the condensate spot on a polished metal plate was proposed at the end of the 19th century by R. Glatzel. In 1908, E. Escat proposed his original device, which, thanks to concentric circles applied to the mirror, made it possible to indirectly estimate the amount of air exhaled through each half of the nose by the size of the fogged area.
The disadvantage of fogging methods is that they only allow the quality of exhalation to be assessed, while the inhalation phase is not recorded. Meanwhile, nasal breathing is usually impaired in both directions and less often only in one phase, for example, as a result of a "valve mechanism" with a mobile polyp of the nasal cavity.
Objectification of the state of the respiratory function of the nose is necessary for a number of reasons. The first of them is the assessment of the effectiveness of the treatment. In some cases, patients continue to complain of difficulty in nasal breathing after treatment, explaining this by the fact that they sleep with an open mouth, their mouth dries out, etc. In this case, we may be talking about the patient's habit of sleeping with an open mouth, and not about unsuccessful treatment. Objective data convince the patient that his nasal breathing is quite sufficient after treatment and it is only a matter of the need to restructure breathing to the nasal type.
In some cases of ozena or severe atrophy of the endonasal structures, when the nasal passages are extremely wide, patients still complain of difficulty in nasal breathing, although the size of the condensation spots on the mirror surface indicates good patency of the nasal passages. As more in-depth studies show, in particular using the rhinomanometry method, the complaints of these patients are caused by extremely low air pressure in the wide nasal passages, the absence of "physiological" turbulent movements and atrophy of the receptor apparatus of the nasal mucosa, which together leads to the patient losing the sensation of the passage of an air stream through the nasal cavity and to a subjective impression of the absence of nasal breathing.
Speaking about simple methods of assessing nasal breathing, one cannot help but mention the "test with a fluff" by V.I. Voyachek, which clearly demonstrates to the doctor and the patient the degree of patency of the nasal passages. Two fluffs 1-1.5 cm long, made of cotton fibers, are simultaneously brought to the nostrils. With good nasal breathing, the excursions of the fluff, set in motion by the flow of inhaled and exhaled air, are significant. With insufficient nasal breathing, the movements of the fluff are sluggish, of small amplitude, or completely absent.
To detect a nasal breathing disorder caused by an obstruction in the nasal vestibule (the so-called anterior nasal valve), the Kottle test is used. It consists of pulling the soft tissues of the cheek outward at the level and near the wing of the nose during calm breathing through the nose, moving the latter away from the nasal septum. If nasal breathing becomes freer, the Kottle test is assessed as positive and the function of the anterior nasal valve is considered impaired. If this technique does not noticeably improve nasal breathing in the presence of objective insufficiency, the cause of the respiratory function disorder of the nose should be sought in deeper sections. The Kottle technique can be replaced by the Kohl technique, in which a wooden splinter or a button probe is inserted into the nasal vestibule, with the help of which the wing of the nose is moved outward.
Rhinomanometry
During the 20th century, many devices were proposed for conducting objective rhinomanometry with the registration of various physical indicators of the air flow passing through the nasal passages. In recent years, the method of computer rhinomanometry has been increasingly used, allowing to obtain various numerical indicators of the state of nasal breathing and its reserve.
The normal nasal breathing reserve is expressed as the ratio between the measured values of intranasal pressure and air flow in different phases of one respiratory cycle during normal nasal breathing. The subject should be sitting in a comfortable position and at rest without any previous physical or emotional stress, even the most minimal. The nasal breathing reserve is expressed as the resistance of the nasal valve to the air flow during nasal breathing and is measured in SI units as kilopascal per liter per second - kPa/(l-s).
Modern rhinometers are complex electronic devices, the design of which uses special micro sensors - converters of intranasal pressure and air flow velocity into digital information, as well as special programs for computer mathematical analysis with calculation of nasal breathing indices, means of graphic display of the parameters under study. The presented graphs show that with normal nasal breathing, the same amount of air (ordinate axis) passes through the nasal passages in a shorter time with two to three times less air flow pressure (abscissa axis).
The rhinomanometry method provides three ways of measuring nasal breathing: anterior, posterior and retronasal manometry.
Anterior rhinomanometry involves inserting a tube with a pressure sensor into one half of the nose through its vestibule, while this half of the nose is excluded from the act of breathing with the help of a hermetic obturator. With the appropriate "corrections" made by the computer program, it is possible to obtain fairly accurate data with its help. The disadvantages of the method include the fact that the output indicator (total nasal resistance) is calculated using Ohm's law for two parallel resistors (as if simulating the resistance of both open halves of the nose), while in fact one of the halves is blocked by the pressure sensor. In addition, as Ph. Cole (1989) notes, changes that occur in the mucovascular system of the nose in patients in the intervals between right- and left-sided studies reduce the accuracy of this method.
Posterior rhinomanometry involves placing a pressure sensor in the oropharynx through the mouth with tightly pressed lips, with the end of the tube placed between the tongue and soft palate so that it does not touch the reflexogenic zones and does not cause a gag reflex that is unacceptable for this procedure. To implement this method, the person being examined must be patient, accustomed, and have no high pharyngeal reflex. These conditions are especially important when examining children.
In retronasal or transnasal rhinomanometry (using the method of F. Kohl, used by him in the children's respiratory department of the hospital in Toronto), a neonatal feeding catheter (No. 8 Fr) with a lateral lead near the tip is used as a pressure conductor, which ensures unimpeded conduction of the pressure signal to the sensor. The catheter, lubricated with lidocaine gel, is passed 8 cm along the bottom of the nasal cavity to the nasopharynx. Minor irritation and anxiety of the child disappear immediately as soon as the catheter is fixed with adhesive tape to the upper lip. Differences in the indicators of the three methods are insignificant and depend mainly on the volumes of the cavities and the aerodynamic characteristics of the air flow at the location of the end of the tube.
Acoustic rhinomanometry. In recent years, the method of acoustic scanning of the nasal cavity to determine some metric parameters related to its volume and total surface has become increasingly widespread.
The pioneers of this method were two scientists from Copenhagen, O. Hilberg and O. Peterson, who in 1989 proposed a new method for examining the nasal cavity using the above principle. Later, the company SRElectronics (Denmark) created a serially produced acoustic rhinometer "RHIN 2000" intended for both everyday clinical observations and scientific research. The device consists of a measuring tube and a special nasal adapter attached to its end. An electronic sound transducer at the end of the tube sends a continuous broadband sound signal or a series of intermittent sound pulses and records the sound reflected from the endonasal tissues, returning to the tube. The measuring tube is connected to an electronic computer system for processing the reflected signal. Contact with the measuring object is made through the distal end of the tube by means of a special nasal adapter. One end of the adapter corresponds to the contour of the nostril; sealing of the contact to prevent "leakage" of the reflected sound signal is carried out using medical petroleum jelly. It is important not to apply force to the tube so as not to change the natural volume of the nasal cavity and the position of its wings. The adapters for the right and left halves of the nose are removable and can be sterilized. The acoustic probe and the measuring system provide a delay in interference and send only undistorted signals to the recording systems (monitor and built-in printer). The unit is equipped with a mini-computer with a standard 3.5-inch disk drive and a high-speed non-volatile disk of permanent memory. An additional disk of permanent memory with a capacity of 100 MB is provided. Graphic display of the parameters of acoustic rhinometry is carried out continuously. The display in the stationary mode shows both single curves for each nasal cavity and series of curves reflecting the dynamics of changing parameters over time. In the latter case, the curve analysis program provides both averaging of curves and display of probability curves with an accuracy of at least 90%.
The following parameters are evaluated (in graphic and digital display): transverse area of the nasal passages, volume of the nasal cavity, difference indicators of areas and volumes between the right and left halves of the nose. The capabilities of the RHIN 2000 are expanded by an electronically controlled adapter and stimulator for olfactometry and an electronically controlled stimulator for carrying out allergic provocation tests and a histamine test by injecting the corresponding substances.
The value of this device is that it allows for precise determination of quantitative spatial parameters of the nasal cavity, their documentation and research in dynamics. In addition, the device provides ample opportunities for conducting functional tests, determining the effectiveness of the drugs used and their individual selection. The computer database, color plotter, storage of the received information in memory with the passport data of the examined, as well as a number of other possibilities allow us to classify this method as very promising both in practical and scientific research terms.
What do need to examine?

