Medical expert of the article
New publications
Atelectasis of the lung: discoid, right, left, upper, lower, middle
Last reviewed: 28.11.2021

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
In clinical pulmonology, the complex of symptoms accompanying the compaction of the parenchyma of the lungs and the absence of air in their gas exchange zone (alveoli and alveolar courses) is called lung atelectasis, that is, the partial expansion of its individual lobes or segments with loss of alveolar functions.
Atelectasis leads to a significant reduction in the respiratory volume and ventilation of the lungs, and with total damage to airborne lung tissue - to respiratory failure with a fatal outcome.
In accordance with ICD-10, this pathological condition has code J98.1.
Epidemiology
According to the American Journal of Respiratory and Critical Care Medicine, atelectasis of the lung after inhalation anesthesia in American surgical patients occurs in 87% of cases, in Canadian patients - in 54-67%. The incidence of this pulmonary complication after an open cardiological operation in developed countries is today 15% with the death rate of patients - 18.5%, which is 2.79% of the total death from complications of surgical interventions.
Over the past 20 years, the number of premature newborns, according to the WHO, is growing steadily throughout the world. Preterm birth (occurring before the 37th week of gestation) is 9.6% per 12.6 million births per year. However, this indicator differs in different regions, with the largest share of preterm labor in Africa (11.8%), and the lowest in Europe (6.3%).
In the United States, respiratory distress syndrome of newborns is among the five most frequent causes of infant mortality and causes 5.6% of deaths.
A congenital atelectasis is responsible for 3.4% of newborn deaths.
Also atelectasis is common in young children, because their airways are narrower, and many structures continue to form.
Causes of the atelectasis of the lung
There is no single cause of lung atelectasis for all varieties of this pathology. Thus, the partial atelectasis (focal, isolated or segmental atelectasis) and the total atelectasis or lung collapse may differ in the size of the affected area - they may have different etiologies.
Explaining the pathogenesis of lung atelectasis, it should be recalled that bronchopulmonary alveoli have the appearance of vesicles separated by connective tissue septums, permeated with a network of capillaries, in which arterial blood is oxygenated (that is, absorbs inhaled oxygen), and venous releases carbon dioxide. With atelectasis, ventilation of part of the lungs is disturbed, the partial pressure of oxygen in the air filling the alveoli falls, which leads to a disruption of gas exchange in the small circle of the circulation.
Pulmonologists determine the types of atelectasis either depending on the specific features of its localization in airway structures - atelectasis of the right lung, atelectasis of the left lung, atelectasis of the lobe of the lung (lower, middle or upper), or taking into account its pathogenesis. For example, primary atelectasis, which is also congenital atelectasis, occurs in newborn infants with anomalies in the opening of the lungs (especially in cases of prematurity); more about it will be discussed later - in the section Atelectasis in newborns.
All other cases are considered to be secondary or acquired conditions, among which obstructive or obturation atelectasis and non-obstructive (including atelectasis compression and distensive) are distinguished.
Since the right middle lobe of the lungs is the narrowest and surrounded by a large volume of lymphoid tissue, atelectasis of the middle lobe of the lung is considered to be the most frequent.
Obturation atelectasis (in most cases partial) is diagnosed when lung collapsing (collapse) occurs as a result of aspiration of the respiratory tract by a foreign body (which blocks the passage of air) or masses coming from gastroesophageal reflux disease; blockage of bronchi by mucous exudate with obstructive bronchitis, severe tracheobronchitis, emphysema, bronchiectasis, acute and chronic eosinophilic and interstitial pneumonia, asthma, etc.
For example, atelectasis with tuberculosis (usually segmental) most often develops with bronchial obstruction by blood clots or caseous masses from caverns; Also, with tuberculosis on the bronchioles, the granulomatous tissue can spread over the tissue.
The stages of total obstructive atelectasis pass into each other with any localization, with a rapid deterioration in the patients' state - as oxygen, carbon dioxide and nitrogen are absorbed in the "blocked" alveoli and the total composition of the blood gases changes.
Dysfunction of the lung tissue, which causes compression atelectasis, is the result of its extrathoracic or intrathoracic compression by hypertrophic lymph nodes, enlarged fibrous neoplasias, large tumors, effusion from the pleura, etc., which leads to a collapse of the alveoli. Specialists often observe atelectasis in lung cancer, localized in the mediastinal region of thymomas or lymphomas, bronchoalveolar carcinoma, etc.
In the case of total lesions of the lung parenchyma, total atelectasis and lung collapse can be diagnosed. When injuries to the chest disrupt its tightness with the ingress of air into the pleural cavity, intense pneumothorax develops with atelectasis (but atelectasis is not synonymous with pneumothorax).
And the so-called discoid or lamellar atelectasis refers to compression, and its name was obtained from the image of the shadow on the X-ray image - in the form of elongated transverse bands.
Distential atelectasis or functional (most often segmental and subsegmental, localized in the lower lobes) is etiologically associated with inhibition of neuron activity in the respiratory center of the medulla oblongata (with trauma and brain tumors, with general inhalation anesthesia conducted through a mask or intubation tube); with a decrease in the functions of the diaphragm in bedridden patients; with increased pressure in the abdominal cavity due to dropsy and increased gas production in the intestine. In the first case, there are iatrogenic causes of atelectasis: with endotracheal anesthesia, the pressure and absorption of gases in the lung tissues change, causing collapsing of the alveoli. As surgeons say, atelectasis is a frequent complication of various abdominal operations.
In some sources, contractile atelectasis (constricting) is produced, which is caused by a decrease in the size of the alveoli and an increase in the surface tension in bronchial spasms, trauma, surgical interventions, and the like.
Atelectasis may be a symptom of a number of interstitial lung diseases that damage the surrounding alveoli of the tissue: exogenous allergic alveolitis (allergic pneumonitis or pneumoconiosis), sarcoidosis of the lungs, bronchiolitis obliterans (cryptogenic pneumonia), desquamative interstitial pneumonia, Langergans pulmonary histiocytosis, idiopathic pulmonary fibrosis, etc.
Risk factors
Risk factors for atelectasis include:
- age is less than three or older than 60 years;
- prolonged bed rest;
- impaired swallowing function, especially in the elderly;
- lung disease (see above);
- broken ribs;
- premature pregnancy;
- cavitary operations under general anesthesia;
- respiratory muscle weakness due to muscular dystrophy, damage to the spinal cord or other neurogenic condition;
- deformities of the chest;
- the use of drugs whose side effects extend to the respiratory system (in particular, hypnotics and sedatives);
- obesity (excessive body mass);
- smoking.
Symptoms of the atelectasis of the lung
The first signs of incomplete lung function are manifested by shortness of breath and a decreased expansion of the chest wall during inspiration.
If the pathological process affected a small area of the lungs, the symptoms of lung atelectasis are minimal and limited to a feeling of lack of air and weakness. When the defeat is significant, the person pales; his nose, ears and fingertips become cyanotic (cyanosis); There are stabbing pains on the side of the lesion (not often). Fever and an increased heart rate (tachycardia) can occur when atelectasis is accompanied by an infection.
In addition, among the symptoms of atelectasis include: irregular fast-paced, superficial breathing; blood pressure drop; coldness of feet and hands; decrease in temperature; cough (without phlegm).
If atelectasis develops on the background of bronchitis or bronchopneumonia, and the lesion is extensive, there is a sudden exacerbation of all symptoms, and breathing becomes rapid, superficial and arrhythmic, often with wheezing.
Symptoms of atelectasis in newborns are manifested by wheezing, moaning exhalation, irregular breathing with apnea, swelling of the nostrils, cyanosis of the face and all skin, drawing the skin in between the ribs - with inspiration (from the development of atelectasis). Also noted are frequent heart rate, lower body temperature, muscle rigidity, convulsions.
Atelectasis in newborns
Atelectasis in newborns or primary atelectasis is the main cause of the so-called respiratory distress syndrome of newborns (ICD-10 code - P28.0-P28.1).
Congenital atelectasis occurs due to obstruction of the respiratory tract with amniotic fluid or aspiration with meconium, which lead to an increase in pressure in the lungs and pleural cavity and damage to the alveolar epithelium. Also, this pathology may be a consequence of intrauterine maldevelopment of lung and bronchial tissue (Wilson-Mikichi syndrome), bronchopulmonary dysplasia (in children born at the gestation period less than 32 weeks), congenital alveolar or alveolar-capillary dysplasia, intrauterine pneumonia, congenital malformation surfactant.
The latter factor is of particular importance in the pathogenesis of congenital atelectasis. Normally, adhesion of the alveolar walls does not occur due to the surfactant produced by the special cells of the basal membrane of the alveoli (alveolocytes of the second type), which possesses surface-active properties (the ability to reduce the surface tension) to the protein-phospholipid substance that covers the alveolar walls from the inside.
Synthesis of the surfactant in the fetal lungs begins after the 20th week of embryonic development, and the child's lung contraceptive system is ready for their spreading at birth only after the 35th week. So any delay or abnormality of fetal development and intrauterine oxygen starvation can cause a surfactant deficiency. In addition, the association of this disorder with mutations in the genes of surfactant proteins SP-A, SP-B and SP-C has been revealed.
According to clinical observations, when endogenous surfactant deficiency develops, dysontogenetic scattered atelectasis with pulmonary parenchyma edema, excessive stretching of the walls of lymphocytes, increased permeability of capillaries and stagnation of blood. Their natural result is acute hypoxia and respiratory failure.
In addition, atelectasis in newborns born before the due date, in cases of placental peeling, perinatal asphyxia, diabetes mellitus in pregnant women, and surgical delivery may be a symptom of the presence on the walls of the alveoli of the coagulated fibers of the fibrillar protein hyaline (hyaline membrane syndrome, lung hyalinosis, endoalveolar hyalinosis of newborns or respiratory distress syndrome of the 1st type). At term infants and young children atelectasis can be provoked by a genetically determined disease, like cystic fibrosis.
Complications and consequences
The main consequences and complications of atelectasis:
- hypoxemia (lowering the level of oxygen in the blood due to a violation of the mechanics of breathing and reducing pulmonary gas exchange);
- decreased blood pH (respiratory acidosis);
- increased load on the respiratory musculature;
- pneumonia from atelectasis (with the development of an infectious inflammatory process in the atelectasized part of the lung);
- pathological changes in the lungs (overstretching of intact lobes, pneumosclerosis, bronchiectasis, cicatricial degeneration of a part of the pulmonary parenchyma, retention cysts in the bronchus zone, etc.);
- asphyxia and respiratory insufficiency;
- narrowing of the lumen of the arterial and venous vessels of the lungs.
Diagnostics of the atelectasis of the lung
To diagnose atelectasis, the doctor records all complaints and symptoms and conducts a physical examination of the patient with auscultation of his lung stethoscope.
To determine the cause, blood tests are needed - general, biochemical, for blood pH and its gas composition, for fibrinogen, antibodies (including Mycobacterium tuberculosis), rheumatoid factor, etc.
Instrumental diagnosis consists of spirometry (determining the volume of the lungs) and pulse oximetry (setting the level of oxygen saturation of the blood).
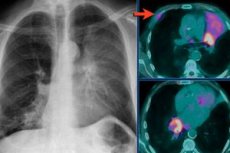
The main diagnostic method for this pathology is chest x-ray in the proximal-distal and lateral projections. A radiograph with atelectasis makes it possible to examine the state of the thoracic organs and see the shadow in the region of atelectasis. At the same time, the image clearly shows the trachea, the heart and the root of the lung, the changes in the intercostal distances and the shape of the arch of the diaphragm deviated towards the side.
It is possible to detect lung atelectasis on CT with high resolution: for visualization and refinement of small details of interstitial lung diseases. High-precision computer images help confirm the diagnosis, for example, of idiopathic pulmonary fibrosis, and avoid the need for a lung biopsy.
Bronchoscopy with atelectasis (with the introduction into the lungs of a flexible bronchoscope through the oral cavity or nose) is performed to examine the bronchi and obtain a small sample of tissue. In addition, bronchoscopy is used for treatment purposes (see below). But if for histological examination you need more pulmonary tissue from a certain zone, identified by x-ray or CT, resort to a surgical endoscopic biopsy.

What do need to examine?
Differential diagnosis
Differential diagnostics performed by X-ray examination of patients is intended to distinguish this pathology from pneumonia, chronic inflammatory process in bronchial tubes, bronchoconstriction in case of infection with tuberculosis infection, pulmonary sequestration, cystic and tumor formations, etc.
Treatment of the atelectasis of the lung
Treatment of atelectasis varies depending on the etiology, duration and severity of the disease at which it develops.
Atelectasis in newborns is treated with a tracheotomy that opens the respiratory tract, respiratory support (positive-pressure breathing apparatus), and the introduction of oxygen. Although high concentrations of oxygen, used for a long time, exacerbate damage to lung tissue and may lead to the development of retrolental fibroplasia in premature infants. In most cases, there is a need for artificial ventilation, which provides oxygenation of the blood in the arteries.
Medications for atelectasis in newborns - surfactant substitutes Infasurf, Survant, Sukrim, Surximax - are injected into the trachea of the child at regular intervals, and the dose is calculated depending on the body weight.
If atelectasis is caused by airway obstruction, then the first cause is eliminated the causes of blockage. This can be the removal of clots by an electric pump or by bronchoscopy (followed by washing the bronchi with antiseptic compounds). Sometimes there is enough postural drainage with a cough: the patient coughs, lying on his side, his head is below the chest, and everything that blocks the airway path comes out with a cough.
Antibiotics are prescribed to fight infection, which almost always accompanies secondary obturation atelectasis - see Antibiotics for pneumonia
In the development of bedridden patients with atenectasis with hypoxia, physiotherapy is performed using constant pressure by inhaling a mixture of oxygen and carbon dioxide; UHF sessions, electrophoresis with drugs. Positive effect is provided by respiratory gymnastics with atelectasis (which increases the depth of breathing and its rhythmicity) and therapeutic massage with lung atelectasis, which allows accelerating the evacuation of exudate.
If the cause of atelectasis is a tumor formation, chemotherapy, radiation and surgical intervention may be necessary. Operative treatment is also used in those cases where, due to necrosis, the affected area of the lung should be removed.
According to doctors, emergency care for atelectasis can be provided only with urgent hospitalization. In a medical setting, patients are injected with strophanthin, camphor, and corticosteroids. To stimulate respiration, drugs from the group of respiratory analeptics can be used, for example, nicotinic acid diethylamide (Nitacamide) - parenterally 1-2 ml to three times a day; drops are taken orally (20-30 drops two or three times a day); Etymisol (in the form of tablets - 50-100 mg three times a day, as a 1.5% solution - subcutaneously or in the muscle). Side effects of both drugs are manifested by dizziness, nausea, increased anxiety and sleep disorders.
Prevention
First of all, the prevention of atelectasis concerns patients who are undergoing an operation under inhalation anesthesia, or which operation is already done. To prevent damage to the lungs, at least 1.5-2 months prior to the planned surgical treatment, quit smoking and increase water intake. And for the operated patients, respiratory gymnastics and a sufficient level of humidity in the rooms are necessary. In addition, doctors do not recommend "lie down" in bed and, if possible, move (at the same time this is a good way to prevent postoperative adhesions).
Also, doctors are strongly advised to properly treat respiratory diseases (especially in children) and prevent them from becoming chronic.
Forecast
A favorable prognosis for the outcome of this pathological condition of the lungs is given by physicians with compression and distal atelectasis. And the result of obturation atelectasis depends on many factors: its causes, the patient's condition, the quality and timeliness of medical care.
As for atelectasis in newborns, to date, the mortality rate of infants with primary atelectasis and respiratory distress syndrome of newborns is 15-16 for every hundred cases.


 [
[